Psychological Disorders
The distressing symptoms of a psychological disorder often go hand in hand with circular thoughts, feelings, and actions. When the symptoms form a recognisable pattern, a medical doctor can diagnose and treat a person.
Diagnosing disorders
The medical diagnosis of a mental health condition is a complex process of matching an individual’s pattern of physical and psychological symptoms to behaviours associated with a disorder, or disorders. Some conditions, such as a learning disability or neuropsychological problems are easily identified. Functional disorders that affect personality and conduct are more difficult, however, as they involve numerous biological, psychological, and social factors.
What are mental health disorders?
Mental health disorders are characterised by the presence of unusual or abnormal mood, thinking, and behaviours that cause an individual significant distress or impairment, and disrupt their ability to function. Impairment occurring as the result of common stressors such as bereavement would not be considered a disorder. Diverse social and cultural factors impacting on behaviours might also rule out the presence of mental health problems.
Disorders can be classified into diagnostic groups (which will be examined on this page) and the two main works used to identify, categorise, and organise them are the World Health Organisation’s International Clarification of Disease (ICD-10) and the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
Assessment of a mental health condition
Clinical diagnosis is only made after a careful assessment process that includes observation and interpretation of a person’s behaviours and discussion with them and, if relevant, their family, carers, and specialist professionals. Putting a name to a person’s distress can help them – and their support systems – gain a deeper understanding of their difficulties, and manage them better, but it can also negatively shape a person’s outlook and contribute to self-fulfilling prophecies.
✔ Physical examination – A doctor will first eliminate physical illness that could be causing symptoms. Medical examination can also reveal intellectual disabilities or speech disorders due to physical abnormalities. Imaging techniques may be used to test for brain injury or dementia, and blood tests can reveal a genetic predisposition to certain disorders.
✔ Clinical interview – If no physical illness is identified, an individual may be referred to a mental health specialist. They will ask the patient about their life experiences, their family history, and recent experiences that relate to their problem. The conversation will also aim to uncover any predisposing factors, strengths, and vulnerabilities.
✔ Psychological tests – Particular aspects of a person’s knowledge, skill, or personality will be evaluated through a series of tests and/or tasks, usually in the form of checklists or questionnaires standardised for use on very specific groups. For example, such tests may measure adaptive behaviours, beliefs about the self, or traits of personality disorder.
✔ Behavioural assessment – A person’s behaviour will also be observed and measured, normally in the situation where their difficulties occur, to gain an understanding of the factors that precipitate and/or maintain their symptoms. The patient might also be asked to make their own observations by recording events in a diary or using a frequency counter.
Depression
This is a common condition that may be diagnosed when a person has been feeling down and worried, and has lost pleasure in daily activities, for more than two weeks.
What is it?
The symptoms of depression can include continuous low mood or sadness, having low self-esteem, feeling hopeless and helpless, being tearful, feeling guilt-ridden, and being irritable and intolerant of others.
A person with depression is unmotivated and uninterested, finds it difficult to make decisions, and takes no enjoyment from life. As a result, the individual may avoid the social events that they normally enjoy, so missing out on social interaction, which can cause a vicious circle which sees them spiralling further downwards.
Depression can make it difficult for a person to concentrate and remember things. In extreme cases the sense of hopelessness may lead to thoughts of self-harm.
Many internal and external factors such as childhood experiences and life events, physical illness, or injury, can cause depression. It can be mild, moderate, or sever and is extremely common – according to the World Health Organisation (WHO) more than 350 million people suffer from it globally.
How is it diagnosed?
A medical doctor can make a diagnosis by asking the person questions about their particular symptoms. One objective is to find out how long the symptoms have been going on. The doctor may also suggest blood tests to rule out any other illness that may cause the symptoms of depression.
Subsequent treatment depends on the severity of the depression, but the main option is to undergo psychotherapy. Antidepressants may be offered to help the person cope with everyday life. For mild to moderate depression, exercise can be helpful. In severe cases, hospital admission or medication for psychotic symptoms may be needed.
Internal and external causes

A wide range of biological, social, and environmental factors can cause depression. External causes predominately encompass life events that can have a negative impact upon a person, and often act in combination with internal causes – those within an individual – to trigger depression.
. External causes:
Money, or the lack of it, and the stress caused by financial concerns and worries about debt.
Stress when a person cannot cope with the demands on them.
Job or unemployment effects status and self-esteem, perception of a positive future, and ability to engage socially.
Bereavement following the death of a family member, or pet.
Alcohol and drugs due to the physiological, social, and economic consequences of addiction.
Bullying among children and adults, whether physical or verbal, face to face or online.
Loneliness as a result of health or disability, especially in the elderly.
Pregnancy and birth and the overwhelming prospect of parenthood for new mothers.
Relationship problems leading to depression in the longer-term.
. Internal causes:
Personality traits, such as neuroticism and pessimism.
Childhood experiences, especially if the person felt out of control and helpless at the time.
Family history, if a parent or sibling has had depression.
Long-term health problems, such as heart, lung, or kidney disease, diabetes, and asthma.
☑ TREATMENT
. Cognitive and behavioural therapies such as behavioural activation, cognitive behaviour therapy, compassion focused, acceptance and commitment, and cognitive therapies.
. Psychodynamic psychotherapy and counselling.
. Antidepressants on their own or alongside therapy.
Bipolar disorder
This condition is characterised by extreme swings – highs (mania) and lows (depression) – in a person’s energy and activity levels, which is why it was originally called manic depression.
What is it?
There are four types of bipolar disorder: bipolar 1 is severe mania lasting for more than a week (the person may need hospitalisation); bipolar 2 causes swings between a less severe mania and low mood; cyclothymia features longer-term hypomanic and depressive episodes lasting for up to two years; and unspecified bipolar disorder, which is a mixture of the three types. During a mood swing an individual can undergo extreme personality changes, which puts social and personal relationships under severe strain.
The main cause of bipolar is commonly believed to be an imbalance of the chemicals in brain function. Known as neurotransmitters, these chemicals include noradrenaline, serotonin, and dopamine, and relay signals between nerve cells, see: Applied Psychology (1). Genetics also play a role: bipolar disorder runs in families, and it can develop at any age. It is thought that two in every 100 people have an episode at some stage; some only have a couple in their lifetime, while others have many. Episodes may be triggered by stress; illness; or hardships in everyday life, such as relationship difficulties or problems with money or work.
How is it diagnosed?
The affected person is assessed by a psychiatrist or clinical psychologist, who asks about the symptoms and when they first occurred. Signals leading up to an episode are explored too. The doctor also looks to eliminate other conditions that can cause mood swings. The individual is usually treated with medication and lifestyle management techniques.
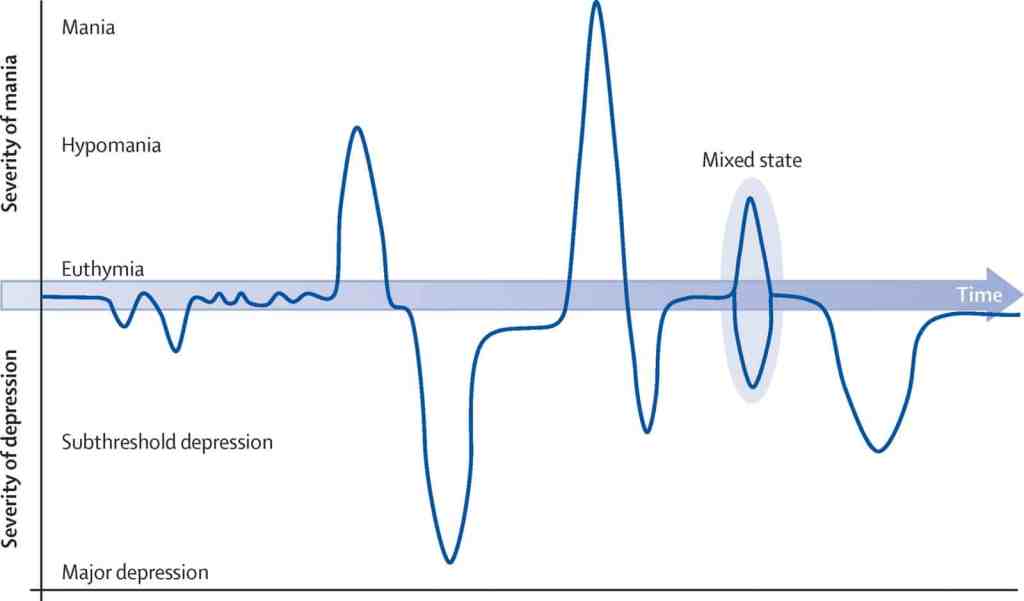
There are distinct phases to the mood swings of bipolar disorder. The extent and timescale of fluctuations and the way moods manifest themselves and affect personality can vary widely.
Balanced/Normal Mood This is a state between episodes in which the person copes with regular daily routines and can plan and predict the consequences of day-to-day actions.
Hypomania In this form of mania, lasting a few days, an individual can be highly productive and function well. It can precede full mania.
Depression The person cannot experience pleasure, has difficulty sleeping, no appetite, may be delusional, hallucinate, and experience disturbed, even suicidal thoughts.
Mania This severe form may last a week or more. Symptoms include hyperactivity, rapid uninterruptable and loud speech, risk-taking, lack of sleep, and inflated self-image.
Mixed State The person suffers from mania at the same time as depression. The individual may, for example, be hyperactive and have depressive symptoms at the same time.
☑ TREATMENT
. Cognitive behavioural therapy
. Lifestyle management including regular exercise, better diet, and sleep routines, which may improve mood regulation; and use of diaries and daily awareness methods, which may help the individual to recognise signs of mood changes.
. Mood stabilisers taken long term to minimise likelihood of mood swings; medication dosage often adjusted during episodes of hypomania, mania, or depression.
Perinatal mental illness
Occurring at any time during pregnancy and up to a year after giving birth, perinatal mental illnesses include PPD (postpartum depression), sometimes called postnatal depression, and postpartum psychosis.
What is it?
Feeling tearful or irritable just after giving birth is so common it is dubbed the “baby blues”, but these feelings only last for a couple of weeks. What sets PPD apart from baby blues is the length of time it lasts. It is a longer-term moderate to severe depression that can develop in new mothers (and occasionally fathers) at any time in the year after birth. Symptoms include constant low mood or mood swings, low energy levels, difficulty bonding with the baby, and frightening thoughts. The individual may cry easily and profusely and feel acutely fatigued yet have sleep problems. Feelings of shame and inadequacy, worthlessness, and fear of failure as a parent are common. In severe cases, panic attacks, self-harm, and thoughts of suicide occur. However, most individuals make a full recovery. Untreated, PPD may last for many months or longer.
PPD can develop suddenly or slowly and is usually caused by hormone and lifestyle changes and fatigue. It is not clear why some people develop PPD, but risk factors appear to include difficult childhood experiences, low self-esteem, a lack of support, and stressful living conditions.
How is it diagnosed?
To determine whether an individual has PPD, a doctor, midwife, or health visitor assesses symptoms using an efficient and reliable screening questionnaire such as the Edinburgh Postnatal Depression Scale, which rates mood and activity levels over the previous seven days. Other assessment scales are used to assess mental wellbeing and functioning.
Good clinical judgement is needed when interpreting the results of these questionnaires as new parents are likely to be less active simply as a result of their new responsibilities.
POSTPARTUM PSYCHOSIS
An extremely serious condition, postpartum psychosis (also known as puerperal psychosis) affects 1–2 women per 1,000 births. It usually occurs in the first few weeks after delivery but may begin up to six months after birth. Symptoms often develop rapidly and include confusion, high mood, racing thoughts, disorientation, paranoia, hallucinations, delusions, and sleep disturbance. The individual may also have obsessive thoughts about the baby. Immediate treatment is needed because of the potentially life-threatening thoughts and behaviours associated with the disorder. Treatment comprises hospitalisation (usually in a highly monitored mother and baby treatment unit), medication (antidepressants and antipsychotics), and psychotherapy.
Range of symptoms
The symptoms of postpartum depression are similar to those of anxiety and general depression. Symptoms can make it difficult to complete day-to-day activities and routines, and can affect an individual’s relationship with their baby, partner, family, and friends. Typically, the symptoms include:
Negative feelings Intense irritability and anger.
Mood Swings Elation followed by enervation.
Depressed Mood Feeling unable or unwilling to cope.
Fatigue Ranging from lethargy to exhaustion.
Withdrawal From partner, family, and friends.
Appetite Loss of appetite or appetite for unhealthy foods.
Apathy Reduced interest in activities that used to bring enjoyment.
Fear Apprehensive about being a good parent.
Crying Excessive crying and feeling tearful.
Difficulty bonding Not feeling expected parental love for baby.
Sleep patterns Inability to sleep or sleeping too much.
☑ TREATMENT
. Cognitive and behavioural therapies in a group, one-to-one, or as guided self-help; one-to-one counselling.
. Lifestyle management, such as talking to partner, friends, and family; resting; regular exercise; and eating healthily and regularly.
. Antidepressants alone or with psychotherapy.
DMDD (disruptive mood dysregulation disorder)
DMDD is a childhood disorder characterised by almost constant anger and irritability combined with regular and severe temper tantrums.
What is it?
DMDD is a recently identified disorder (2013) that children with a history of chronic irritability and serious temper outbursts are now recognised as having. The child is sad, bad tempered and/or angry almost every day. The outbursts are grossly out of proportion with the situation at hand, occur several times every week, and in more than one place (at home, school, and/or with peers). Strained interactions that occur only between a child and their parents, or a child and their teacher, do not indicate DMDD.
How is it diagnosed?
For a diagnosis of DMDD, the symptoms must be evident consistently for more than a year and interfere with a child’s ability to function at home and at school. One cause can be that the child misinterprets other people’s expressions, in which case training in facial-expression recognition can be offered. Diagnosed children are generally under the age of 10, but not younger than six or older than 18. One to three per cent of children under the age of 10 have symptoms.
Disruptive behaviour
Children with DMDD regularly have severe temper tantrums, inconsistent with their developmental stage, three or more times a week in at least two different settings. Typical behaviour includes destroying things or throwing things around the room, shouting abuse at teachers, peers, or parents, and being angry and irritable almost all of the time.
Children with DMDD were once identified as having paediatric bipolar disorder, but they do not present with the episodic mania or hypomania of that disorder. They are unlikely to develop bipolar but are at higher risk of depression and anxiety as adults.
☑ TREATMENT
. Psychotherapy for both child and family to explore emotions and develop mood management techniques.
. Lifestyle management including positive behaviour support to establish better communication and minimise outburst triggers.
. Antidepressants or antipsychotics to support psychotherapy.
SAD (seasonal affective disorder)
SAD is a form of seasonal depression linked to changing levels of light that typically starts in autumn as the days shorten. It is also known as “winter depression” or “hibernation state”.
What is it?
The nature and severity of SAD vary from person to person, and for some it can have a significant impact on their day-to-day life. Typically, the symptoms come and go with the seasons, and always begin at the same time of year, often in the autumn. Symptoms include low mood, a loss of interest in everyday activities, irritability, despair, guilt, and feelings of worthlessness. People with SAD lack energy, feel sleepy during the day, sleep for longer than normal at night, and find it hard to get up in the morning. As many as one in three people are affected.
SAD’s seasonal nature can make diagnosis difficult. Psychological assessment looks at a person’s mood, lifestyle, diet, seasonal behaviour, thought changes, and family history.
Seasonal cause and effect
Sunlight level affects a part of the brain called the hypothalamus and alters the production of two chemicals: melatonin (which controls sleep) and serotonin (which changes mood).
Secretion of melatonin by the pineal gland is triggered by darkness/inhibited by light and controlled by the hypothalamus.
Summer pattern
. Melatonin drops so person has more energy.
. Serotonin production increases, improving mood and outlook.
. Sleep is good, but not excessive, so person has more energy.
. Diet improves as cravings subside.
. Improved energy results in increased activity and more social contact.
Winter pattern
. Melatonin increases so person is tired and wants to sleep.
. Serotonin production drops, causing person to feel low.
. Desire to stay in bed and sleep can lead to reduced social contact.
. Craving carbohydrates can cause overeating and weight gain.
. Constant daytime fatigue affects work and family life.
☑ TREATMENT
. Psychotherapies, such as cognitive behavioural therapy and counselling.
. Lifestyle management by improving access to light – sitting near windows when inside, using a sunlight-simulating light bulb at the correct level of lux, and daily outdoor activity.
Panic disorder
Panic attacks are an exaggerated reaction to the body’s normal response to fear or excitement. With panic disorder, a person regularly experiences such attacks for no obvious reason.
What is it?
The normal reaction to fear or excitement causes the body to produce the hormone adrenaline to prepare for “fight or flight” from the source of fear. If a person has a panic attack, apparently normal thoughts or images trigger the brain’s fight-or-flight centre, resulting in adrenaline racing around the body causing symptoms such as sweating, increased heart rate, and hyperventilation. Attacks last about 20 minutes and can be very uncomfortable.
The individual may misinterpret these symptoms, saying they feel as if they are having a heart attack. The fear can further activate the brain’s threat centre, so more adrenaline is produced, worsening symptoms.
Individuals who have recurring panic attacks can fear the next one so much that they live in a constant state of “fear of fear”. Attacks may, for example, be set off by fear of being in a crowd or a small space, but often they are triggered by internal sensations that have nothing to do with the outside world. As a result, everyday tasks can become difficult and social interactions daunting. Those with panic disorder may avoid certain places or activities, so the problem persists because the person can never “disconfirm” their fear.
What are the causes?
One in ten people suffer from occasional panic attacks; panic disorder is less common. Traumatic life experiences, such as a bereavement, can trigger the disorder. Having a close family member with panic disorder is thought to increase the risk of developing it. Environmental conditions such as high carbon dioxide levels may cause attacks. Some illnesses, for example an overactive thyroid, can produce similar symptoms to panic disorder, and a medical doctor will rule such illnesses out before making a diagnosis.
Constant cycle of anxiety and fear
A person perceives a threat and starts to panic. The physical symptoms develop, worsening the anxiety and therefore the symptoms, which in turn increase the likelihood of a repeat attack.
✔ SYMPTOMS OF A PANIC ATTACK
The symptoms result from the action of the autonomic nervous system – the part not under conscious control.
Increased heart rate Adrenaline causes the heart to pump faster to move blood containing oxygen to where it is needed. This can result in chest pains.
Feeling faint Breathing is faster and shallower to increase oxygen, causing hyperventilation and light-headedness.
Sweating and pallor Sweating increases to cool the body. The person may also become pale as blood is diverted to where it is needed most.
Choking sensation Faster breathing feels like choking – oxygen level rises but not enough carbon dioxide is exhaled.
Dilated pupils The pupil (black part of the eye) becomes dilated to let in more light, making it easier to see to escape.
Slowed digestion As digestion is not crucial for “flight”, it slows. The sphincters (valves) relax, which makes the sufferer feel nauseous.
Dry mouth The mouth can feel very dry as body fluids are concentrated in the parts of the body where they are most needed.
☑ TREATMENT
. Cognitive behavioural therapy to identify triggers, prevent avoidance behaviour, and learn to disprove feared outcomes.
. Support groups to meet others with the disorder and get advice.
. Selective serotonin reuptake inhibitors (SSRIs)
Specific phobias
A phobia is a type of anxiety disorder. Specific phobias manifest themselves when a person anticipates contact with, or is exposed to, the object, situation, or event they fear.
What are they?
Specific, simple phobias (as opposed to the complex ones, agoraphobia, and claustrophobia) are the most common psychological disorders in children and adults. A phobia is much more than fear and arises when a person develops an exaggerated or unrealistic sense of danger about a situation or object. The fear may not make any sense, but the individual feels powerless to stop it. Anticipated or actual exposure (even to an image) can cause extreme anxiety or a panic attack. Symptoms include rapid heart rate, breathing difficulties, and a feeling of being out of control.
A combination of genetics, brain chemistry, and other biological, psychological, and environmental factors can give rise to a phobia. It can often be traced back to a frightening event or stressful situation a person either witnessed or was involved in during early childhood. A child can also “learn” a phobia through seeing other family members demonstrate phobic behaviour.
Specific phobias often develop during childhood or adolescence and may become less severe with age. They can also be associated with other psychological conditions such as depression, obsessive compulsive disorder, and post-traumatic stress disorder.
How are they diagnosed?
Many affected individuals are fully aware of their phobia, so a formal diagnosis is not necessary, and they do not need treatment – avoiding the object of their fear is enough to control the problem. However, in some people habitual avoidance of a feared object can also maintain or worsen the phobia, and seriously impact aspects of their lives. A patient can be referred to a specialist with expertise in behavioural therapy.
Types of specific phobia
There is a wide variety of objects or situations that can trigger a phobia. Specific, so-called simple, phobias fall into five groups: blood-injection-injury, natural environment, situational, animal, and “other” types. With the exception of the first type, specific phobias are two to three times more common in females than males.
Blood-injection-injury A unique group of phobias in which the sight of blood or needles causes a vasovagal reaction (a reflex action that slows down the heart rate, reducing blood flow to the brain) that can result in fainting. Unlike all other phobias, this is as common in males as it is in females.
Natural Environment A person with a phobia from this group has an irrational fear of a natural event, which they often associate with imagery of potentially catastrophic outcomes. Examples include storms, deep water, germs, and fear of heights, such as being near a cliff edge.
Situational These are phobias of being in a specific situation, which can range from visiting the dental surgery to stepping into an old lift, flying, driving over a bridge or through a tunnel, or getting into a car.
Animal This group of phobias includes insects, snakes, mice, cats, dogs, and birds, among other animals. It could be rooted in a genetic predisposition for survival from animals that were a threat to human ancestors.
Other Phobias Thousands of people are tormented by an array of phobias, including the fear of vomiting; a specific colour, for example anything that is yellow or red (including foodstuffs); the number 13; the sight of a belly button or toes; sudden loud noises; fancy dress characters, such as clowns; trees; or contact with cut flowers.
☑ TREATMENT
. Cognitive behavioural therapy to overcome a phobia using a system of graded steps to work towards the goal of confronting the feared object or situation without fear; anxiety management techniques to master each step.
. Mindfulness to raise tolerance of anxiety and thoughts or images associated with the distress.
. Anti-anxiety medication or antidepressants alongside therapy if the phobia is impairing day-to-day living.
Agoraphobia
This is an anxiety disorder characterised by a fear of being trapped in any situation in which escape is difficult or rescue is unavailable if things go wrong.
What is it?
Agoraphobia is a complex phobia that is not, as many think, simply a fear of open spaces. The individual dreads being trapped and avoids whatever triggers the terror of being unable to escape. The result can be a fear of travelling on public transport, being in an enclosed space or crowd, going shopping or to health appointments, or leaving the house. The associated panic attack brought on by such an experience is accompanied by negative thoughts – for example, the person may think that as well as being trapped they are going to look ridiculous, because they are out of control in public. The symptoms, or fear of them, are disruptive and result in avoidance behaviours that make leading a normal life hard.
Agoraphobia can develop if an individual has a panic attack, then worries excessively about a repeat experience. In the UK, one-third of those who have panic attacks go on to develop agoraphobia. Biological and psychological factors are the probable cause. Experiencing or witnessing a traumatic event, mental illness, or an unhappy relationship may play a part.
Treatment can help – about one-third are cured and 50 per cent find that symptoms improve. Other conditions are first excluded by a medical doctor that may be causing the symptoms.
Types of symptoms
The symptoms of agoraphobia are classified into three types: the physical symptoms that a person experiences in the feared situation; behavioural patterns associated with the fear; and cognitive symptoms – the thoughts and feelings a person has anticipating or living with the fear. The combination can make it difficult for a person to function day to day.
Physical Rapid heart and breathing rate, chest pain, dizziness, shaking, feeling nauseous, and breathing problems.
Behavioural Excessive planning to avoid crowds, queues, and public transport, or not going out at all or only with a trusted person.
Cognitive Predictions of shaming by others, over-thinking potential disasters, catastrophic thoughts of being trapped or injured, and feeling out of control.
☑ TREATMENT
. Intensive psychotherapy such as cognitive behavioural therapy to explore the thoughts that maintain the phobia; behavioural experiments to gather evidence that defuses strongly held beliefs.
. Self-help groups using safe visual material to work on exposure to the feared situation; teaching how to manage a panic attack by breathing slowly and deeply.
. Lifestyle management such as exercise and a healthy diet.
Claustrophobia
An irrational fear of being trapped in a confined space or even the anticipation of such a situation, claustrophobia is a complex phobia that can cause extreme anxiety and panic attacks.
What is it?
For a person with claustrophobia, being confined induces physical symptoms similar to those of agoraphobia (above). The fear also increases negative thoughts of running out of oxygen or suffering a heart attack with no chance of escape. Many individuals also experience feelings of dread and fear of fainting or losing control.
Claustrophobia may be caused by conditioning following a stressful situation that occurred in a small space. This might be traced back to childhood, when, for example, an individual was confined in a tiny room or was bullied or abused. The condition can also be triggered by unpleasant experiences at any stage of life, such as turbulence on a flight or being trapped in a lift. The individual fears a repeat of being confined as well as overimagining what could happen in a small space. As a result, they plan their daily activities carefully to minimise the likelihood of “becoming trapped”.
Sometimes claustrophobia is observed in other family members, which suggests a genetic vulnerability to the disorder and/or a learned associated response.
☑ TREATMENT
. Cognitive behavioural therapy to re-evaluate negative thoughts through exposure to the feared situation in small steps, so the individual realises that the worst fear does not occur.
. Anxiety management to cope with anxiety and panic by using breathing techniques, muscle relaxation, and visualising positive outcomes.
. Anti-anxiety medication or antidepressants prescribed in extreme cases.
GAD (generalised anxiety disorder)
People with this disorder experience continual unrestrained and uncontrollable worry (even when no danger is present), to the extent that day-to-day activity and functioning can become impaired.
What is it?
An individual with GAD worries excessively about a wide range of issues and situations. Symptoms include “threat” reactions such as heart palpitations, trembling, sweating, irritability, restlessness, and headaches. GAD can also cause insomnia and difficulty in concentrating, making decisions, or dealing with uncertainty.
The person may become obsessed with perfectionism, or with planning and controlling events. The physical and psychological symptoms can have a debilitating effect on social interactions, work, and everyday activities, leading to lowered confidence and isolation. Worries may revolve around family or social matters, work, health, school, or specific events. A person with GAD experiences feelings of anxiety most days, and as soon as they resolve one worry another appears. They overestimate the likelihood of bad or dangerous things happening and predict the worst possible outcome. The individual may even report positive beliefs about the helpfulness of worry, such as: “Worrying makes it less likely that bad things will happen”. Long-term or habitual avoidance of fearful situations or places compounds the disorder because the individual never gathers evidence that their fears are unfounded, so maintaining the worry.
Women are 60% more likely to develop GAD than men.
Balancing worries
Anxiety becomes a problem when a person is weighed down with worries for the majority of days in a six-month period, or longer.
☑ TREATMENT
. Cognitive behavioural therapy to identify triggers, negative thoughts, habitual avoidance, and safety behaviours.
. Behavioural therapy to identify new behavioural goals, with achievable steps.
. Group therapy with assertiveness training and building self-esteem to help counteract unhelpful beliefs and unfounded fears.
Social Anxiety Disorder
Individuals with this condition experience an overwhelming fear of being judged or of doing something embarrassing in social situations. The disorder can cause disabling self-consciousness.
What is it?
An individual with social anxiety disorder (also called social phobia) experiences excessive nerves or dread of social situations. They may be anxious only in specific circumstances, such as speaking or performing in public, or experience distress in all social situations.
The person tends to be extremely self-conscious and worries about others evaluating them negatively. They dwell on past social incidents, obsessing about how they might have come across. Social anxiety causes the person to overplan and rehearse for anticipated situations, which may lead to odd or awkward behaviour. Individuals may then gather evidence to support their fears, because difficult situations often arise as a result of the person’s anxiety or over-rehearsal.
This disorder leads to isolation and depression and can seriously affect social relationships. It can also have a negative impact on performance at work or school.
Symptoms before social interaction The individual may prepare and rehearse excessively in advance, planning topics of conversation or how to present themselves in a specific way.
During interaction Physical symptoms such as trembling, rapid breathing, racing heart, sweating, or blushing occur as the body’s “fight or flight” system is activated. In extreme cases, the person may experience a panic attack.
After interaction The person conducts a detailed, negative, and self-critical appraisal of the social situation, dissecting conversations and body language and giving them a negative slant.
☑ TREATMENT
. Cognitive behavioural therapy to recognise and change negative thought patterns and behaviours.
. Group therapy for the opportunity to share problems and practise social behaviour.
. Self-help including affirmations, rehearsing before social events, and using video feedback to disprove negative assumptions.
Separation anxiety disorder
This anxiety disorder can develop in children whose natural concern about being separated from their parent, primary caregiver, or home persists beyond the age of two years.
What is it?
Separation anxiety is a normal adaptive reaction that helps to keep babies and toddlers safe while they attain competence to cope with their environment. However, it can be a problem if it persists for more than four weeks and interferes with age-appropriate behaviour.
The child becomes distressed when they need to leave a primary carer and fears that harm will come to that person. Situations, such as school and social occasions can also be a trigger. Affected children may experience panic attacks, disturbed sleep, clinginess, and inconsolable crying. They may complain of physical problems such as stomach-ache, headache, or just feeling unwell for no apparent reason. Older children may anticipate feelings of panic and struggle to live and travel independently.
Separation is the most common anxiety disorder in children under 12 years old. It can also affect older children, and it may be diagnosed in adulthood. The disorder can develop after a major stressor such as the loss of a loved one or pet, moving home, changing school, or parents’ divorce. Overprotective or intrusive parenting can contribute.
Separation anxiety is very treatable with behavioural therapies that include building planned separations into times of the day when the person is feeling least vulnerable.
Being alone
Worries about losing their primary carer are common and the child may relive their daytime fears in nightmares. They may refuse to sleep alone or suffer from insomnia.
Vivid fears – The child worries excessively about being detached from their primary carer – even if only in a separate room.
Unwanted burden – Anxious feelings may manifest themselves as physical pains as the child struggles to fix their panic of separation into something tangible.
☑ TREATMENT
. Cognitive behavioural therapy for anxiety management; assertiveness training for older children and adults.
. Parent training and support to promote and reinforce short periods of separation that are then extended gradually.
. Anti-anxiety medication and antidepressants for older individuals in combination with environmental and psychological interventions.
Selective mutism
This is an anxiety disorder in which people are unable to talk in certain social situations but are able to speak at other times. It is usually first recognised between the ages of three and eight years.
What is it?
Selective mutism is associated with anxiety, and children who are affected by it struggle with excessive fears and worries. They are generally able to speak freely where they feel comfortable but are unable to talk in specific situations, when they do not engage, go still, or have a frozen facial expression when expected to talk. This inability to speak is not the result of a conscious decision or a refusal.
The mutism can be triggered by a stressful experience, or it can stem from a speech or language disorder, or hearing problem, which makes social situations involving communication particularly stressful. Whatever the cause, everyday activities are difficult as are relationships within the family, nursery, or school. Treating the condition can prevent it persisting into adulthood – the younger the child is when diagnosed the easier it is to treat.
If symptoms persist for more than a month, the child should be seen by a medical doctor, who can refer them for speech and language therapy. A specialist will ask whether there is a history of anxiety disorders, a likely stressor, or a hearing problem. Treatment depends on how long the child has had the condition, the presence of learning difficulties or anxieties, and the support that is available.
State of fear
Children with selective mutism literally “freeze” when they are expected to talk and make little or no eye contact. The condition is more common in children who are learning a second language.
☑ TREATMENT
. Cognitive behavioural therapy using positive and negative reinforcements to build speech and language skills; graded exposure to specific situations to reduce anxiety, removing pressure on the child to speak.
. Psychoeducation can provide information and support for parents and carers; relieve general anxiety; and reduce chances of the disorder persisting into adulthood.
OCD (obsessive compulsive disorder)
This is a debilitating anxiety-related condition characterised by intrusive and unwelcome obsessional thoughts that are often followed by repetitive compulsions, impulses, or urges.
What is it?
OCD is often marked by thoughts that reflect an excessive sense of responsibility for keeping others safe and an overestimation of the perceived threat an intrusive thought signifies. OCD is clinical and often starts with an obsessional thought, which the person focuses on, in turn raising anxiety levels. Checking everything is in order and following rituals can provide relief, but the distressing thought returns. The obsessive thoughts and compulsions are time-consuming and individuals may struggle to function day to day or have a disrupted social or family life. The disorder may be triggered by an event in the person’s history that they felt highly responsible for. Family history, differences in the brain, and personality traits also play a part. An examination of thoughts, feelings, and behaviour patterns determines OCD, but its similarity to other anxiety disorders can make diagnosis difficult.
With pure OCD, a person has intrusive and disturbing thoughts about harming people, but rather than performing observable compulsions, their compulsions take place in the mind.
OBSESSIONS (THOUGHTS)
Fear of causing harm Excessive attention paid to thoughts about actions that could cause harm.
Intrusive thoughts Obsessive, repetitive, and even disturbing thoughts about causing harm.
Fear of contamination Thinking that something is dirty or germ-ridden and will cause illness or death to the person or someone else.
Fear related to order or symmetry Concern that harm could result unless tasks are done in a specific order.
COMPULSIONS (BEHAVIOURS)
Rituals Following rituals such as counting or tapping to prevent harm and provide relief from the cycle of fear.
Constant checking Examining household appliances, lights, taps, locks, windows (to counter fear of causing harm by fire), driving routes (fear of having run a person over), or people (fear of upsetting someone).
Correcting thoughts Trying to neutralise thoughts to prevent disasters.
Reassurance Repeatedly asking others to confirm everything is OK.
☑ TREATMENT
. Cognitive behavioural therapy involving exposure to triggers and learning how to control responses.
. Anti-anxiety medication and/or antidepressants to help relieve symptoms of depression and anxiety.
. Specialist residential treatment in addition to therapy and medication for extremely severe cases of OCD.
Hoarding disorder
Also known as compulsive hoarding, this disorder is characterised by the excessive acquisition of, and/or the inability or unwillingness to dispose of, large quantities of objects.
What is it?
An individual with hoarding disorder does not discard worn-out possessions, for fear of either needing them again or of something bad happening to other people if they get rid of anything. The person stores sentimental items as they believe that discarding them will stop emotional needs being met. The individual continues to accumulate items even when space is running out. Hoarding can be hard to treat because the person does not see it as a problem and experiences such overwhelming discomfort at reducing the clutter that they avoid doing so. Alternatively, the person may be aware of the problem but too ashamed to seek help or advice.
Hoarding disorder may begin as a way of coping with a stressful life event. Hoarding may be part of other disorders such as OCD, depression, or psychotic disorders. In medical assessment, the doctor questions the person about their feelings on acquiring objects and their overestimation of responsibility for causing harm by discarding items.
Living with hoarding
A person with hoarding disorder may let junk mail, bills, receipts, and heaps of paper pile up. The resulting clutter can pose a health and safety risk and makes it hard to move from room to room, which is distressing for the individual and affects their, and their family’s, quality of life. This may lead to isolation and impaired or difficult relationships with other people.
☑ TREATMENT
. Cognitive behavioural therapy to examine and weaken the thoughts that maintain the hoarding behaviour and allow adaptive or flexible alternatives to emerge.
. Lifestyle management at home to motivate reducing clutter for health and safety reasons.
Antidepressants to decrease the associated anxiety and depression.
BDD (body dysmorphic disorder)
In this condition a person has a distorted perception of how they look. The individual typically spends an excessive amount of time worrying about their appearance and how others view them.
What is it?
BDD is an anxiety disorder that can have a huge impact on daily life. An individual with BDD worries obsessively about how they look. They often focus on a specific aspect of their body, for example, viewing a barely visible scar as a major flaw or seeing their nose as abnormal, and are convinced that others view the “flaw” in the same way. The person may spend a great deal of time concealing an aspect of their appearance, seeking medical treatment for the part of the body believed to be defective, and/or diet or exercise excessively.
BDD affects about one in every 100 people in the UK, can occur in all age groups, and is seen in males and females in equal numbers. It is more common in people with a history of depression or social anxiety disorder, and it often occurs alongside OCD or GAD (see above). BDD may be due to brain chemistry or genetics and past experiences may play a role in triggering its development. In medical assessment, the doctor asks the person about their symptoms and how they affect them and may refer them to a mental health specialist for further treatment.
Breaking the cycle
Treatment for BDD can be highly successful and focuses on breaking the cycle of thoughts, feelings, and behaviours that maintain it. The length of time treatment takes depends on the severity of the condition.
Consider a person with a negative self-image. The cycle starts with a trigger and moves towards efforts to change appearance.
Trigger Seeing their reflection, misinterpreting body language, or someone’s passing comment can start the cycle.
Automatic Thoughts Negative thoughts dominate, for example, “I am defective, defective people are worthless, so I am worthless”.
Low Mood The perceived constant social threat leads to chronic anxiety and depression.
Efforts To Change Appearance Safety behaviours or social avoidance prevail. The person may apply excessive make-up or use clothing to conceal the perceived defective attribute; seek cosmetic surgery; use extreme diet and exercise to change body shape; and avoid social situations, so increasing feelings of isolation.

☑ TREATMENT
. Cognitive behavioural therapy to identify self-appraisal related to the problem body part and weaken the beliefs that maintain it.
. Antidepressants and anti-anxiety medication alongside therapy.
Illness anxiety disorder
Previously known as hypochondria, this condition involves a person worrying excessively about becoming seriously ill, even if thorough medical examinations reveal nothing.
What is it?
Hypochondria is considered to be two separate conditions: illness anxiety disorder if there are no symptoms or they are mild, or somatic symptom disorder, if there are major physical symptoms causing emotional stress. People with illness anxiety disorder become excessively preoccupied with their health. Some have exaggerated feelings about an existing condition (about 20 per cent do have heart, respiratory, gastrointestinal, or neurological problems). Others experience unexplained symptoms. They convince themselves that these symptoms indicate a serious illness that has been missed by medical professionals and their teams.
Illness anxiety is a long-term condition that fluctuates in severity and may worsen with age or stress. It can be triggered by a major life event. Someone who is anxious or depressed is more prone to the disorder. Assessment and treatment focus on stopping avoidance and reassurance behaviours, re-evaluating health beliefs, and increasing the person’s tolerance of uncertainties.
Endless checks
Disbelief in medical opinion reaffirms the person’s anxiety and results in extra focus on the body part or illness, which causes panic and physical symptoms. Safety behaviours, such as avoiding situations for fear of exposure to disease, and reassurance from others provide brief respite.
Typically, there is a pain or sensation which instigates the trigger. The person then misinterprets the signs by being convinced they have a serious illness. They then research that illness extensively. Frequent body checks and possible avoidance measures are made, despite a medical doctor and other medical professionals finding no sign of illness.
☑ TREATMENT
. Behavioural therapies such as attention training to stop a person over-attending to body sensations and help re-evaluate beliefs.
. Antidepressants prescribed alongside therapy.
PTSD (post-traumatic stress disorder)
This is a severe anxiety disorder that may develop any time after a person experiences or witnesses a terrifying or life-threatening event, or series of events, over which they have little or no control.
What is it?
PTSD is seen in people who have been in military combat or a serious incident, or suffered prolonged abuse or the unexpected injury or death of a family member. The event itself activates the fight-or-flight reflex in the brain and body, putting the person on hyperalert to deal with the consequences of the trauma and protect them from a repeat of the episode. An individual with PTSD feels that the threat remains, so their heightened response is maintained, causing an array of unpleasant symptoms including panic attacks, involuntary flashbacks, nightmares, avoidance and emotional numbing, anger, jumpiness, insomnia, and difficulty concentrating. These symptoms usually develop within a month of the event (but may not appear for months or years) and last for more than three months. PTSD can lead to other mental health problems and excessive alcohol and drug use is common.
Watchful waiting is advisable at first to see if the symptoms subside within three months as treatment too early can exacerbate PTSD.
Brain changes
PTSD is a survival reaction. The symptoms result from an aim to help survive further traumatic experiences and include raised levels of stress hormones and other changes in the brain:
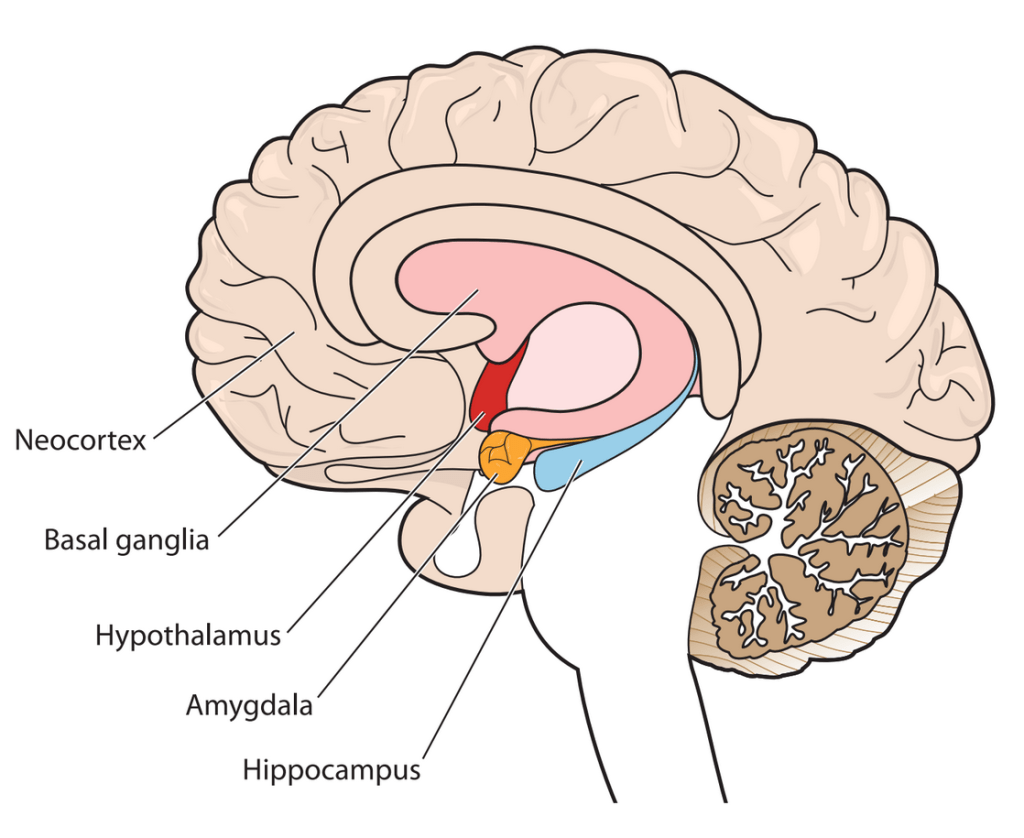
Hippocampus – PTSD increases stress hormones, which reduce activity in the hippocampus and make it less effective in memory consolidation. Both the body and mind remain hyperalert because its decision-making ability is reduced.
Prefrontal cortex – Trauma affects the function of the prefrontal cortex, changing behaviours, personality, and complex cognitive functions such as planning and decision-making.
Hypothalamus – In PTSD, the hypothalamus sends signals to the adrenal glands (on the kidneys) to release the hormone adrenaline into the bloodstream and increase the chances of survival.
Amygdala – PTSD increases the function of the amygdala, activating the fight-or-flight response and increasing sensory awareness.

☑ TREATMENT
. Trauma-focused therapy such as cognitive behaviour therapy, or eye movement desensitisation and reprocessing, to help reduce the sense of current threat by working on memory of the event.
. Compassion-focused therapy to self-soothe from shame-based thoughts and images. Group therapy for vulnerable groups such as war veterans.
ASR (acute stress reaction)
Also called acute stress disorder, ASR can appear quickly after an exceptional physical or mental stressor such as bereavement, road traffic incident, or assault, but does not usually last long.
What is it?
Symptoms of ASR are anxiety and dissociative behaviour following exposure to a traumatic and unexpected life event. The person may feel disconnected from themselves, have difficulty handling emotions, suffer mood swings, become depressed and anxious, and may have panic attacks. They often experience difficulty sleeping, poor concentration, and recurrent dreams and flashbacks, and may avoid situations that trigger memories of the event. Some individuals have psychological symptoms such as raised heart rate, breathlessness, excessive sweating, headaches, chest pain, and nausea.
ASR is described as acute because the symptoms come on fast, but do not usually last. Symptoms of ASR can begin within hours of the stress and are resolved within a month; if they last longer, they may turn into PTSD (see above).
ASR may resolve without therapy. Talking things over with friends or relatives can help those with the disorder understand the event and put it into context. Individuals may benefit from psychotherapies too.
Anecdotal evidence suggests that 80% of people with ASR develop PTSD 6 months later.
How does ASR differ from PTSD?
ASR and PTSD are similar, but the timeframes are different. The symptoms of ASR occur within a month of an event, and they usually resolve within the same month. The symptoms of PTSD may or may not develop within a month of the event or events. PTSD is not diagnosed unless the symptoms have been evident for more than three months. There is an overlap between what the symptoms are. However, in ASR symptoms involve feelings, such as dissociation, depression, and anxiety, predominate. With PTSD the symptoms relate to a prolonged or persistent response to the fight-or-flight mechanism. There is a higher risk of ASR developing in a person who has had PTSD or mental health issues in the past, and ASR can lead to PTSD.
☑ TREATMENT
. Psychotherapies such as cognitive behavioural therapy to identify and re-evaluate thoughts and behaviours that maintain anxiety and low mood.
. Lifestyle management including supportive listening and stress-relieving practices such as yoga or meditation.
. Betablockers and antidepressants to ease physical symptoms in combination with psychotherapy.
Adjustment disorder
This is a short-term, stress-related psychological disorder that can follow a significant life event. Typically, a person’s reaction is stronger, or more prolonged, than expected for the type of event.
What is it?
Any stressful event can trigger anxiety, difficulty sleeping, sadness, tension, and inability to focus. However, if an individual finds an event especially hard their reaction can be stronger and persist for months. In a child, the disorder can follow family conflicts, problems at school, and hospitalisation. The child may become withdrawn and/or disruptive and complain of unexplained pain or illness. Adjustment disorder is not the same as PTSD or ASR as the stress trigger is not as severe. It normally resolves within months as a person learns how to adapt to a situation and/or the stressor is removed. There is no way to predict whether one person is more likely to develop adjustment disorder than another. It is a result of how they respond to an event and their personal history.
A medical doctor first assesses whether an individual’s symptoms may be due to another condition, such as ASR, before referring them for a psychological assessment.
Causes and outcome
Some life events are known to lead to adjustment difficulties of varying severity. Examples are the death of a friend or family member, divorce or relationship breakdown, moving home, illness or injury, financial worries, or job stress.
. Symptoms begin within 3 months The onset can be traced to an event and symptoms are more severe than expected. They include defiant, impulsive behaviour, sleeplessness, crying, feeling sad and hopeless, anxiety and muscle tension.
. Symptoms resolve in 6 months With a further three months of therapy and the removal of the stressor, a person can learn to turn negative thoughts into healthy actions, to change how they respond to stress.
☑ TREATMENT
. Psychotherapies such as cognitive behavioural therapy, and/or family or group therapies to help identify and respond to stressors.
. Antidepressants to lessen symptoms of depression, anxiety, and insomnia alongside a psychotherapy.
Reactive attachment disorder
This disorder can result in children who do not bond with a caregiver in infancy. Unidentified reactive attachment disorder can be a precursor to lifelong impaired personal development.
What is it?
Attachment theory states that developing a strong emotional and physical bond with a primary caregiver is key to a child’s healthy personal development. Without such a bond a child can become increasingly detached, withdrawn, and distressed, and the physical symptoms relating to stress become obvious.
Persistent disregard of a child’s basic physical needs, frequent changes of primary caregivers, and childhood abuse can disrupt a child’s ability to form social and emotional bonds. The child can develop markedly disturbed ways of relating socially and may be unable to initiate or respond to social interactions.
Disinhibited responses, such as a disregard for convention and impulsive behaviour, used to be included in the medical assessment of this disorder, but these are now considered as a separate diagnosis of disinhibited social engagement disorder.
Associated disorders
Undiagnosed reactive attachment disorder is an underlying factor in a number of psychological problems that emerge in childhood or adulthood under clinical assessment:
. Depression This can develop because a person with reactive attachment disorder sees a constant disparity between expectation and reality.
. Learning difficulties Social isolation creates a hostile environment that can make an individual more likely to have developmental disorders.
. Low self-esteem Without any positive reciprocal interactions in infancy, neutral or negative ones can predominate later, which can affect self-esteem.
. Relationship issues Not developing healthy attachments in childhood makes it difficult to form meaningful relationships in adulthood.
. Social difficulties If a person feels different from their peers, they can be disruptive and are more susceptible to isolation or bullying.
. Substance abuse Individuals who have suffered a disrupted infancy or childhood commonly seek support through drugs.
Long-term impact
Early neutral, negative, or even hostile environments are likely to have a long-term negative impact and affect a person right through to adulthood. An individual’s ability to maintain and make healthy relationships in later life is severely compromised. Reactive attachment disorder can develop in early infancy and the vulnerability it creates is associated with a wide range of disorders that affect both children and adults.
☑ TREATMENT
. Cognitive and behavioural therapies to examine habitual appraisals; dialectical behaviour therapy to help severely affected adults; family therapy to promote good communication; anxiety management, and positive behaviour support.
ADHD (attention deficit hyperactivity disorder)
This neurodevelopmental disorder is diagnosed in children with behavioural symptoms (inattentiveness, hyperactivity, and impulsivity) that are inconsistent with their age.
What is it?
This is a condition that makes it difficult for a child to sit still and concentrate and it is usually noticeable before the age of six. The effects of ADHD can persist into adolescence and adulthood. Adults may also be diagnosed with the pre-existing condition, when persistent problems in higher education, employment, and relationships reveal it. However, the symptoms may not be as clear as they are in children. The level of hyperactivity decreases in adults with ADHD, but they struggle more with paying attention, impulsive behaviour, and restlessness.
The evidence for what causes ADHD is inconclusive, but it is thought to include a combination of factors. Genetics may play a part, which explains why it runs in families. Observations of brain scans also indicate differences in brain structure and have identified unusual levels of the neurotransmitters dopamine and noradrenaline. Other possible risk factors include premature birth, low birthweight, and exposure to environmental hazards. The condition is more common in people with learning difficulties. Children with ADHD may also display signs of other conditions such as ASD, tic disorders or Tourette’s, depression, and sleep disorders. Surveys have shown that worldwide this condition affects more than twice as many boys as girls.
Identifying ADHD
A medical doctor in general practice cannot officially diagnose ADHD, but if they suspect the child has the disorder, they refer them for specialist assessment. The child’s patterns of hyperactivity, inattention, and impulsive behaviour are observed over a six-month period before a treatment plan is prepared.
Hyperactivity
. Difficulties sitting still The child cannot stay seated (or quiet) in situations where it is expected, such as the classroom.
. Constant fidgeting The child may twitch limbs, torso, and/or head, whether sitting or standing.
. Lack of volume control The child shouts and makes loud noises during normal everyday activities.
. Little or no sense of danger This may result in the child running and climbing in environments where these behaviours are neither safe nor appropriate.
Inattentiveness
. Concentration difficulties This causes the child to make errors of judgment and mistakes. Alongside constant movement, this can cause injury.
. Clumsiness The child is prone to dropping and breaking things.
. Easily distracted The child appears not to be listening and is unable to complete tasks.
. Poor organisational skills The child’s inability to concentrate has an impact on organisational abilities.
. Forgetfulness This results in the child losing things.
Impulsivity
. Interrupting The child disrupts conversations regardless of the speaker or situation.
. Inability to take turns The child is unable to wait their turn in conversations and games.
. Excessive talking The child may change a topic often or focus obsessively on one.
. Acting without thinking The child is unable to wait in line or keep up with group pace.
MANAGING ADHD
There are a number of ways that parents can help their child to handle the condition.
. Create predictable routines to calm an ADHD sufferer. Timetable daily activities and keep them consistent. Make sure school timetables are clearly set out too.
. Set clear boundaries and make sure the child knows what is expected of them; praise positive behaviour straightaway.
. Give clear instructions, either visual or verbal, whichever the child finds easier to follow.
. Use an incentive scheme, for example, have a star/points chart whereby a child can earn privileges for good behaviour.
☑ TREATMENT
. Behavioural therapies to help the child and their family manage day to day; psychoeducation for families and carers.
. Lifestyle management such as improving physical health and reducing stress to calm the child.
. Medication can calm (not cure) the person so that they are less impulsive and hyperactive. Stimulants increase dopamine levels and trigger the area of the brain involved in concentration.
ASD (autism spectrum disorder)
ASD describes a spectrum (range) of lifelong disorders that affect a person’s ability to relate to other people and their emotions and feelings, making social interaction difficult.
What is it?
ASD is generally diagnosed in childhood and can present in a variety of ways. A parent or carer may notice that a baby does not use vocal sounds, or an older child has problems with social interaction and non-verbal communication. Symptoms such as repetitive behaviours, problems talking, poor eye contact, tidying or ordering rituals, bizarre motor responses, repetition of words or sentences, a restricted repertoire of interests, and sleep problems are common. Some children with ASD may also have depression.
Genetic predisposition, premature birth, fetal alcohol syndrome, and conditions such as muscular dystrophy, Down’s syndrome, and cerebral palsy are known to be associated with ASD. A medical doctor in general practice first examines the child to rule out physical causes for the symptoms, then refers them for specialist diagnosis. Information is gathered about all aspects of the child’s behaviour and development, at home and school. There is no cure, but specialised therapies such as speech therapy and physical therapy can help. One in every 100 people in the UK has ASD and is identified in more boys than girls.
Degrees of ASD
ASD manifests itself in different ways and to different degrees in each person. Autistic author and academic Stephen M. Shore said, “If you’ve met one individual with autism, you’ve met one individual with autism”.
HIGH FUNCTIONING AUTISM AND ASPERGER’S
High functioning autism (HFA) and Asperger’s Syndrome (AS) are both terms that are applied to people with characteristics of ASD, but who are of above average intelligence with an IQ of more than 70. However, they exist as two separate diagnoses, as those with HFA have delayed language development, which is not present in AS. Diagnoses of HFA or AS may be missed in children as they are socially awkward with a manner that is not easily understood. The ASD traits they share of perfectionism and obsessive interest in a particular subject can mean that they become expert in their area of interest. Like ASD, those with HFA or AS also require strict routines, have sensitivities to certain stimuli, awkwardness, and difficulty behaving appropriately and communicating in social situations; the severity of these symptoms will differ in each person. Long-term difficulties arise with social and intimate relationships, both at school and into adulthood.
Communication: Problems with language are common. Some people with ASD are fluent, while others are speech impaired. All tend to be literal and have difficulty with understanding humour, context, and inference.
Social interaction: Impaired social skills mean that a person with ASD cannot recognise another’s personal space or read body language. The person might think out loud or repeat what another person has said.
Repetitive behaviour: Repetitive behaviour traits are common. An individual may make repetitive movements such as hand flapping or rocking, or develop rituals such as lining up certain toys or flicking switches on and off.
Sensory skills: Heightened sensitivity to sound can cause a person to develop avoidance behaviours such as humming, covering their ears, or self-isolation in a preferred space to escape noise.
Motor skills: Difficulties with movement, such as coordination and motor planning, are common in children with ASD. Fine motor skills like handwriting may also be affected, which can hinder communication.
Perception: Impaired sensory and visual perception means that those with ASD miss non-verbal cues, can be unaware of lies, and usually have difficulty seeing a situation from another person’s perspective.
Hans Asperger, Austrian paediatrician, and researcher of autism, said of ASD: “In science or art, a dash of autism is essential.”
☑ TREATMENT
. Specialist interventions and therapies can assist in areas such as personal safety, hyperactivity, and sleep difficulties.
. Educational and behavioural programmes can support the learning of social skills.
. Medication can help with associated symptoms – melatonin for sleep problems, SSRIs for depression, and methylphenidate for ADHD.
Schizophrenia
This is a long-term condition that affects the way a person thinks. It is characterised by feelings of paranoia, hallucinations, and delusions, and impacts significantly on a person’s ability to function.
What is it?
The word schizophrenia comes from the Greek, and literally means “split mind”, which has led to the myth that people with the condition have split personalities, but they do not. Instead, they suffer from delusions and hallucinations that they believe are real. There are different types of schizophrenia. The main ones are Paranoid (hallucinations and delusions), Catatonic (usual movements, switching between being very active and very still), and Disorganised, which has aspects of both. Despite popular beliefs, individuals with schizophrenia are not always violent. They are however more likely to abuse alcohol and drugs and it is these habits, combined with their condition, that can cause them to become aggressive.
Schizophrenia appears to result from a combination of physical, genetic, psychological, and environmental factors. MRI scans have identified abnormal levels of neurotransmitters dopamine and serotonin and unusual brain structure, and there might be a correlation between the condition and pregnancy or birth complications. It is also thought excessive cannabis use in young adulthood can be a trigger.
Popular theories regarding the causes of schizophrenia in the second half of the twentieth century included family dysfunction theories, such as the “double bind” (when people are faced with contradictory, irreconcilable demands for courses of action), high levels of parent/carer “expressed emotion” (not tolerating those with the disorder) and learning the schizophrenic role through labelling. Since then, mental health specialists have observed that hearing voices or feeling paranoid are common reactions to trauma, abuse, or deprivation. Stress can trigger acute schizophrenic episodes and learning to recognise their onset can help with management of the condition.
How is it diagnosed?
Schizophrenia is diagnosed through clinical interviews and specialist checklists during which the symptoms will be assessed. The earlier the condition is diagnosed, and treatment begun, the better, so that there is less time for its extreme impact on personal, social, and work life to build up. While schizophrenia is not curable, people can overcome it enough to function day to day. A personalised treatment plan that caters to the specific needs of the individual with schizophrenia is required for people with such a complex mental health issue.
Around 1.1% of the global adult population have schizophrenia.
Symptoms of schizophrenia
These are classified as positive or negative. Positive symptoms are psychotic additions to an individual while negative symptoms can look like the withdrawal or flat emotions seen with depression. Schizophrenia is likely if a person has experienced one or more symptoms from both domains for most of the time for a month.
Positive symptoms (psychotic)
These symptoms are classified as positive because they are additions to a person’s mental state and represent new ways of thinking and behaving that only develop with the condition:
. Hearing voices is common and can occur occasionally or all the time. The voices may be noisy or quiet, disturbing, or negative, known, or unknown, and male or female.
. Hallucinations involve seeing things that are not there, but seem very real to the person, and are often violent and very disturbing.
. Feeling sensations can cause a person to be convinced that they have unpleasant creatures such as ants crawling on or under their skin.
. Smelling and tasting things that cannot be identified can arise, and there may be difficulty discriminating between smells and tastes.
. Delusions – fixed beliefs – are held despite evidence to the contrary. The person may think they are famous and/or being chased or plotted against.
. Feelings of being controlled by, for example, a religious or dictatorial delusionist, can overwhelm a person. The beliefs can make them act differently.
Negative symptoms (withdrawal)
These symptoms are called negative because they represent a loss of certain functions, thoughts, or behaviours that a healthy person exhibits, but that are absent in those with schizophrenia:
. Difficulty communicating with others can result in changed body language, a lack of eye contact, and incoherence.
. “Flattened” emotions result in a significantly reduced range of response. The person will take no pleasure in activities.
. Tiredness may result in lethargy, change in sleep patterns, staying in bed, or sitting in the same place for long periods.
. Absence of willpower or motivation makes it difficult or even impossible for a person to engage in normal day-to-day activity.
. Poor memory and concentration mean that the individual is unable to plan or set goals and has difficulty keeping track of thoughts and conversations.
. Inability to cope with everyday tasks results in disorganisation. The individual stops looking after themselves, domestically or personally.
. Becoming withdrawn from social and community activities can disrupt the individual’s social life.
☑ TREATMENT
. Community mental health teams such as social workers, occupational therapists, pharmacists, psychologists, and psychiatrists work together to develop ways to help a person stay stable and progress.
. Medication in the form of antipsychotics is prescribed to reduce monthly positive symptoms, but it does not cure the condition.
. Cognitive behavioural therapy and the technique of reality testing can help with management of symptoms such as delusions. New developments use imagery to defuse stress that negative symptoms cause.
. Family therapy can improve relationships and coping skills within the family and educate anyone in a person’s care.
Anecdotal evidence suggests 1% of the population is likely to develop schizoaffective disorder.
Schizoaffective disorder
This is a long-term medical health condition in which a person suffers both the psychotic symptoms of schizophrenia and the deregulated emotions that characterise bipolar disorder at the same time.
What is it?
While symptoms may vary from person to person, one episode will feature both psychotic and mood symptoms (manic, depressive, or both) for part of the time and a period with only psychotic or mood symptoms for most of the time over a period of at least two weeks.
Schizoaffective disorder can be triggered by traumatic events that took place when a person was too young to know how to cope or was not being cared for in a way that made it possible to develop coping skills. Genetics may play a part, too. It is more common in women and usually begins in early adulthood.
A mental health professional will assess the symptoms and want to know how long they have been present, and what triggers them. This chronic condition impacts on every aspect of a person’s life, but symptoms can be managed. Family interventions to raise awareness of the disorder can improve communication and support.
The different forms
People with this disorder experience periods of psychotic symptoms, such as hallucinations or delusions, with mood disorder symptoms – either of a manic type or a depressive type, but sometimes both. The condition features cycles of severe symptoms followed by periods of improvement.
Psychotic symptoms
. Hallucinations Hearing voices and seeing things that are not there.
. Delusions False, fixed beliefs in things that are not true.
Mood disorder symptoms
. Manic type is hyperactive, feels high, cannot sleep, and takes risks.
. Depressive type feels sad, empty, and worthless.
. Mixed type has symptoms of both depression and mania.
☑ TREATMENT
. Medication is needed long term, usually combinations of mood stabilisers plus antidepressants for depressive types or antipsychotics for manic types.
. Cognitive behavioural therapy can help a person make links between thoughts, feelings, and actions; learn the cues preceding behaviour change; and develop coping strategies.
Catatonia
An episodic condition that affects both behaviour and motor skills, catatonia is characterised by abnormal psychomotor functioning and extreme unresponsiveness when awake.
What is it?
Catatonia is a state of immobility that can persist for days or weeks. Those with the condition may have an extremely negative outlook and may not respond to external events, become agitated, have difficulty speaking due to extreme anxiety, and refuse to eat or drink. Symptoms also include feelings of sadness, irritability, and worthlessness, which can occur nearly every day. An individual may lose interest in activities, lose or gain weight suddenly, have trouble getting to sleep or out of bed, and feel restless. Decision-making is impaired and suicidal thoughts are common.
This condition can have a psychological or neurological cause and may be associated with depression or psychotic disorders. It is estimated that 10–15 per cent of people with catatonia also have symptoms of schizophrenia, while about 20–30 per cent of individuals with bipolar disorder may experience catatonia – mostly during their manic phase.
Diagnosing catatonia
A mental health professional observes an individual and looks for a number of symptoms. At least three out of the 12 symptoms described (below) must be present to confirm a diagnosis of catatonia:
Mutism Silent and apparently unwilling or unable to speak.
Echolalia Constantly repeats what other people have said.
Grimacing Makes distorted facial expressions that show disgust, dislike, and even pain.
Stupor Immobile, lacks expression, and does not respond to stimuli.
Catalepsy May be rigid, have a seizure, or be completely unresponsive in this trance-like state.
Waxy flexibility Limbs can be moved by someone else and will remain in the new position.
Agitation Movement may be purposeless and risky.
Mannerism Strikes poses or makes idiosyncratic movements.
Posturing Moves from one unusual position to another.
Stereotypy Frequent, persistent, repetitive movements.
Negativism Resistant to any outlook rather than a negative one.
Echopraxia Constantly mimics other people’s movements.
☑ TREATMENT
. Medication prescribed depends on the symptoms, but includes antidepressants, muscle relaxers, antipsychotics, and/or tranquillisers such as benzodiazepines, but these carry a risk of dependency. Outside help is needed to ensure compliance with medication and to teach living skills.
. Electroconvulsive therapy may be used when medication is ineffective. This involves transmitting an electric current through the person’s brain.
Delusional disorder
This is a very rare form of psychosis that causes a person to experience complex and often disturbed thoughts and delusions that are not true or based on reality.
What is it?
Previously known as paranoid disorder, delusional disorder is marked by an individual’s inability to distinguish what is real from what is imagined. The delusions may be the misrepresentations of experienced events and are either not true or highly exaggerated. They may be non-bizarre and relate to situations that could occur, such as being followed, poisoned, deceived, or loved from a distance, or be bizarre delusions that are impossible, for example, a belief in an imminent alien invasion.
Delusional disorder can make it hard for a person to concentrate, socialise, and live a normal life, as it can cause dramatic changes in a person’s behaviour that result in conflict with those around them. Individuals may become so preoccupied with their delusions that their lives are disrupted. However, others continue to function normally and, apart from the subject of their delusion, do not behave in an obviously odd manner. Some people experience hallucinations – seeing, hearing, tasting, smelling, or feeling things that are not really there.
Psychological disorders known to trigger delusional episodes include schizophrenia, bipolar disorder, severe depression or stress, and lack of sleep. General medical conditions that can cause them are HIV, malaria, syphilis, lupus, Parkinson’s, multiple sclerosis, and brain tumours. Substances such as alcohol or drug misuse can also trigger delusional episodes in some people.
How is it diagnosed?
A medical doctor in general practice will first take a complete medical history of the individual. They will ask about symptoms and want to know how a delusion affects a person’s day-to-day functioning, any family history of mental health conditions, and details of medications and/or illegal substances a person has been taking.
Thematic delusions
Delusions are fixed beliefs that do not change, even when a person is presented with conflicting evidence, and characteristically follow particular themes (below). Individuals are likely to display the delusion for a month or longer and most do not admit they are problematic. The person may appear completely normal as long as an outsider does not touch on the belief.
Somatic – A person with these delusions has physical or bodily sensations, for example as a result of believing insects are crawling under their skin.
Erotomanic – A delusion in which a person believes that another individual, often someone famous, is in love with them; may lead to stalking behaviour.
Grandiose – An individual with grandiose delusions believes they have a great unrecognised talent or knowledge, for example they may be a special messenger, guru, or God.
Persecutory – A person with these delusions feels that they are being persecuted or mistreated, for example, stalked, drugged, spied on, or the victim of slander.
Jealous – People with this delusion have a morbid, but unfounded belief that their partner has been unfaithful or is deceiving them.
Mixed or unspecified – Themes are said to be mixed if several types of delusion are present, but no particular one dominates. In some cases, the delusion does not fall into any of the main categories and is unspecified.
☑ TREATMENT
. Medication prescribed may include antipsychotic drugs to reduce the delusional symptoms and antidepressants such as selective serotonin reuptake inhibitors (SSRIs) to help with the depression that can be associated with the disorder.
. Psychotherapies such as cognitive behavioural therapy to help examine the strongly held beliefs and support changes needed.
. Self-help groups and social support to reduce the stress that results from living with this disorder and to help those around them, and family, social, and/or school intervention to help develop social skills to reduce the impact of the disorder on quality of life.
Dementia
This is an (as yet) incurable, degenerative disorder, also known as mild or major neurocognitive impairment. It is characterised by memory disorders, personality changes, and impaired reasoning.
What is it?
The term dementia describes a set of symptoms that affect the brain and gradually become more severe. Symptoms include difficulties with concentration, problem-solving, carrying out a sequence of tasks, planning, or organising, as well as general confusion.
A person with dementia may lose track of days or dates and find it hard to follow a conversation or recall the right word for something. They may also be unable to judge distances or see objects in three dimensions. Dementia may cause people to feel insecure and lose their self-confidence and can result in depression.
Many different conditions, such as Alzheimer’s, cardiovascular disease, Lewy bodies, and disorders of the front and side lobes of the brain, cause the symptoms. Dementia is mainly seen in older adults, but it can occur in people in their 50s (known as early onset), and sometimes even younger.
There is no single assessment for dementia. A medical doctor in general practice uses memory and thinking tests and may order a scan to confirm which areas of the brain are damaged. Treatment aims to alleviate symptoms and slow down their progression.
Anecdotal evidence suggests statistically that more than 30% of people over the age of 65 develop dementia.
Causes
. Alzheimer’s disease causes abnormal proteins to build up around brain cells and damage their structure. This disrupts the chemical messages that pass between the cells, so the cells gradually die. Symptoms progress as more parts of the brain are affected.
. Vascular dementia can result from cardiovascular disease. It occurs when blood flow to the brain is impaired (for example, by a stroke) causing problems with reasoning, planning, judgment, and memory.
. Mixed dementia results when Alzheimer’s and vascular dementia occur at the same time.
. Dementia with Lewy bodies has similar symptoms to Alzheimer’s and Parkinson’s disease. Also known as Pick’s disease, it occurs when protein bodies form on nerve cells and often cause hallucinations and delusions.
. Fronto-temporal dementia is a rarer form that affects the temporal (side) and frontal lobes of the brain. It alters personality and behaviour and makes use of language difficult.
How it affects a person
As every person is different their experience of dementia is too. The diagnosis is based on a person’s history and how the symptoms affect their ability to cope day to day.
People with dementia feel insecure, lose confidence in themselves, and need help preparing for the road ahead.
Motor skills – If the areas of the brain responsible for movement are damaged, muscle control lessens.
Emotions – Inability to control or express feelings can cause low self-esteem and depression.
Social skills – The inability to concentrate and follow conversation can make it difficult to relate to people.
Decision-making – Memory loss, poor concentration, and confusion can make decision-making hard or impossible.
Concentration – Lack of focus can make daily routines and independent living very difficult.
Memory – Short-term memory is affected first, but long-term memory also fails as the disease progresses.
Speech – Speaking and control of language become hard, which can be disconcerting for others.
Judgment – No longer feeling in control or able to plan anything leads to loss of faith in own judgment.
Empathy – Struggling to make sense of what is happening leaves little room for thinking of others.
☑ TREATMENT
. Cognitive stimulation and reality orientation therapy for short-term memory.
. Behavioural therapy to help carry out daily routines.
. Validation therapy – the main carer reading out loud, respectful statements.
. Cholinesterase inhibitors to boost memory and judgment.
CTE (chronic traumatic encephalopathy)
Also known as post-concussion syndrome, this is a degenerative condition of the brain characterised by physiological and psychological disturbances following closed head injuries.
What is it?
CTE is most often seen in service personnel or people who take part in high-impact contact sports, such as football, rugby, or boxing, and there is no cure. Physical symptoms include headache, dizziness, and pain. Psychological symptoms are memory loss, confusion, impaired judgment, impulse-control problems, and even hallucinations. An individual may become aggressive and have difficulty maintaining relationships. Signs of Parkinson’s and dementia can emerge later. The disturbances may develop early or emerge years after the head trauma. A preventive approach is advisable, with use of protective head gear and the introduction of rules that disallow contact above chest or shoulder height in sport.
At the moment it is only possible to diagnose CTE after death. Tests, scans, and biomarkers are being developed to help identify the condition earlier.
Cumulative effect of head injury
Multiple blows to the unprotected skull can lead to irreversible injury. In a study of 100 people with mild head injury, 20–50 showed symptoms of CTE three months after the initial injury and about one in 10 still had problems a year later.
[1] A blow to a healthy brain can cause concussion but a person is likely to recover completely.
[2] The initial injury can leave a vulnerability, so the brain is less able to recover from a second blow.
[3] After three or more blows the brain is more susceptible to widespread, permanent damage.
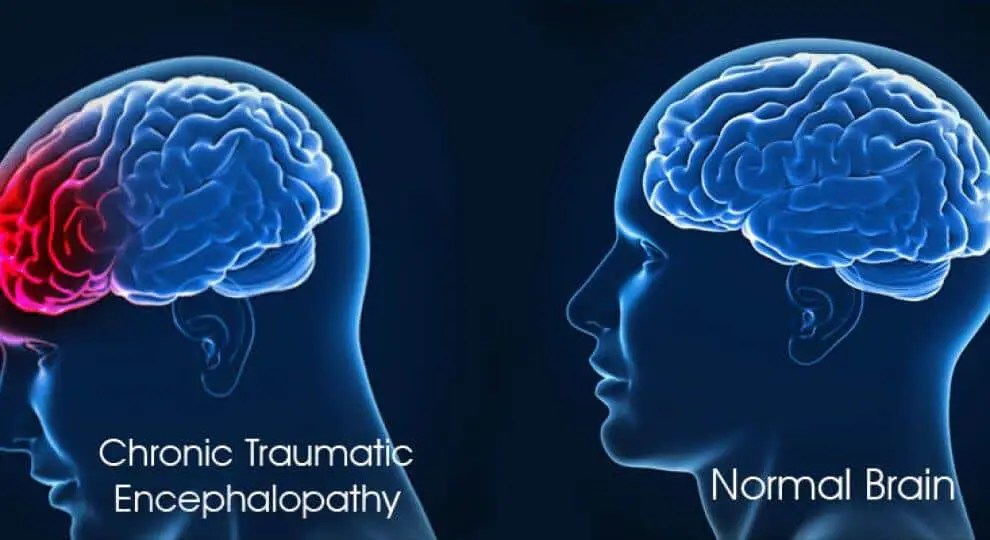
☑ TREATMENT
. Psychotherapies such as cognitive behavioural therapy and mindfulness-based stress reduction.
. Lifestyle management including rest and recuperation after initial head injury followed by a gradual return to activities, stopped if symptoms return.
. Antidepressants if psychological symptoms warrant them.
Delirium (acute confusional state)
This is an acutely disturbed state of mind characterised by lethargy, restlessness, delusions, and incoherence, which can result from a variety of causes including illness, poor diet, or intoxication.
What is it?
Delirium can have a serious impact on day-to-day life, but it is usually short term. An individual has difficulty concentrating and may be confused as to where they are. They may move more slowly or quickly than usual and experience mood swings. Other symptoms include not thinking or speaking clearly, difficulty sleeping or feeling drowsy, reduced short-term memory, and loss of muscle control.
Delirium may occur at any age but is more common in the elderly and can be confused with dementia. It is generally a short-term physical or emotional problem, but it can be irreversible. It is also possible to have dementia and delirium at the same time.
Causes vary, but likely reasons are a medical condition, such as a chest or urinary tract infection, or metabolic imbalance, such as low sodium. Delirium can also follow serious illness, surgery, pain, dehydration, constipation, poor nutrition, or a change in medication.
How is it diagnosed?
A medical doctor in general practice checks the symptoms and assesses movement, cognitive processes, and speech. Some practitioners use observational methods to diagnose or rule out delirium, by watching the person’s behaviour over an entire day. Physical tests may be carried out to check for underlying illness.
Up to 50% of elderly patients in hospital suffer delirium. There are three types:
Hypoactive delirium The person is lethargic and withdrawn, sleepy, unmoving, and hardly reacts to their environment. This type of delirium can easily be mistaken for depression.
Hyperactive delirium The person is agitated, restless, and easily startled. They may experience hallucinations (seeing things that are not there) and delusions (believing things that are not true).
Mixed delirium An individual can have hyper- and hypoactive delirium in the same day. The person may feel they are not in control and have out-of-body sensations.
☑ TREATMENT
. Reality orientation therapy, involving the use of repeated visual and verbal orientation cues delivered in a respectful manner, to help the person understand their surroundings and situation.
. Lifestyle management including routine and scheduled activity with exercise to minimise confusion and help the individual regain some day-to-day control.
. Antibiotics prescribed if illness is identified as the cause, together with hydration if necessary.
Substance use disorder
This is a serious condition in which the use of alcohol or drugs, or both, leads to physical and psychological problems that affect the individual’s working or home life for the worse.
What is it?
Also known as drug use disorder or substance abuse, this condition can cause wide-ranging impairments and psychological distress. Symptoms and signs of substance abuse (whether alcohol or drugs) include taking drugs regularly, maybe daily, to function; taking drugs even when alone; continuing to use drugs even when the person knows it is harming their own health, family, or work; making excuses to use drugs and reacting with aggression to enquiries about their substance use; being secretive about using drugs; losing interest in other activities; impaired ability to work; neglecting to eat or attend to physical appearance; confusion; lethargy; depression; financial problems; and criminal activity such as stealing money.
In the longer term, overconsumption of alcohol can cause weight gain and high blood pressure, and increase the risk of depression, liver damage, problems with the immune system, and some cancers. Drugs can be associated with mental health issues such as depression, schizophrenia, and personality disorders.
Alcohol or drug abuse usually begins as a voluntary behaviour, encouraged, or tolerated within the person’s social and cultural climate. Peer pressure, stress, and family dysfunction can escalate the problem. A child with a family member who has chemical-dependency issues may be at a higher risk of the disorder for either environmental or genetic reasons or both.
How is it diagnosed?
Diagnosis begins with the person recognising that they have a problem, as denial is a common symptom of addiction. Empathy and respect are more likely to induce a person to accept that they have substance use disorder than through orders and confrontation. A medical doctor or specialist grades the person’s behaviour (below) while the individual is using the substance.
Behaviour patterns
The diagnosis of this disorder, whatever the substance, is based upon a set of 11 behaviours related to its use. The severity of the disorder is based on how many of these behaviours are present: 0–1 = no diagnosis; 2–3 = mild substance use disorder; 4–5 = moderate substance use disorder; 6+ = severe substance use disorder.
Impaired control
[1]. Uses substance for longer and/or in larger amounts than originally intended.
[2]. Wants to cut down but cannot do so.
[3]. Spends longer and longer getting, using, and recovering from using the substance.
[4]. Has intense cravings for the substance, which makes it difficult for the person to think about anything else.
Social impairment
[5]. Continues to use despite knowing the problems it causes with life at home or work.
[6]. Continues to use despite arguments with the family or the loss of friendship it causes.
[7]. Gives up social and recreational activities as a result, so spends less time with friends and family, and becomes increasingly isolated.
Risky use
[8]. While under the influence, engages in risky sexual behaviour or puts themselves or others in danger, for example, by driving, operating machinery, or swimming.
[9]. Continues to use while aware that the substance is making psychological or physical problems worse (for example, drinking even when liver damage has been diagnosed).
Pharmacological criteria
[10]. Becomes tolerant of the substance, so needs increasing amounts to achieve the same effects. Different drugs vary in terms of how quickly tolerance develops.
[11]. Suffers withdrawal such as nausea, sweating, and shaking if the intake is stopped.
According to the World Drug Report 2017, for the United Nations Office on Drugs and Crime, 29.5million people in the world have drug use disorder.
☑ TREATMENT
. Psychotherapies, such as cognitive behavioural therapy or acceptance and commitment therapy, to look at the thinking and behaviours that maintain the addiction and change a person’s relationship with their thoughts.
. Psychosocial support through attending meetings with peer groups, such as Alcoholics Anonymous, to motivate and encourage a person to stop substance abuse and improve their quality of life.
. Residential inpatient units in severe cases to limit a person’s activities during detoxification and provide medication necessary to help manage any extreme withdrawal symptoms.
Impulse-control and addiction
Impulse-control disorders are diagnosed in people who cannot withstand the urge to perform problematic behaviours. In addition, a pleasurable activity becomes compulsive and interferes with daily life.
What are they?
The basic concepts underlying impulsive and addictive behaviours overlap. Some psychologists think that impulse-control disorders should be classed as addictions.
In impulse-control disorders, a person perpetuates their behaviour regardless of the consequences, and they become less and less able to control their inner urges. Usually, a person feels an increasing tension or arousal before the action, pleasure or relief while doing it, and regret or guilt in the aftermath. Environmental and neurological factors play a part in the development of the disorders, and they may be triggered by stress.
The recognised impulse-control disorders are compulsive gambling, kleptomania, pyromania, hair pulling, and intermittent explosive disorder. Sex, exercise, shopping, and Internet addictions share similar traits.
| DISORDER | WHAT IS IT? | TREATMENT |
| Intermittent Explosive Disorder | Tendency to short but violent outbursts even though there is no real trigger for the behaviour. | Impulse-control training to identify cues and change responses; adapt environment. |
| Sex Addiction | Intense focus on sex and how to obtain it, regardless of the negative impact on everyday life. | Psychotherapies can support the development of alternative emotional coping strategies. |
| Exercise Addiction | Uncontrollable compulsion to exercise beyond health needs that can result in injury or illness. | Behavioural therapy to manage stress with more adaptive activities and planned exercise. |
| Shopping Addiction | Stress-triggered, irresistible urge to shop, followed by euphoria that provides only temporary relief. | Behavioural therapy to support changes in thinking and responses to break the cycle. |
| Computer/ Internet Addiction | Preoccupation that leads to more time spent online, and mood problems if that time is restricted. | Behavioural therapy to become aware of problem and develop ways to cope with the real world. |
Gambling disorder
Also known as compulsive gambling, this is an impulse-control disorder that exists when a person repeatedly gambles despite the significant problems or distress it causes themselves and others.
What is it?
The thrill of winning releases dopamine from the reward centre in the brain. For some people the act of gambling becomes addictive, and they need ever big wins to achieve the same thrill.
Once a gambling disorder takes hold, the cycle is difficult to break. The disorder may start from desperation for money or a desire for easy money, the need to experience the highs, the status associated with success, and the atmosphere of a gambling environment. The person can become irritable if they attempt to cut down, then gamble because of the distress. Severe disorders can take hold through a financial desperation to recoup lost money. Increasing the size of stakes is common. Even when the person finally wins again, it is rarely enough to cover losses. Aside from significant financial loss, excessive gambling can impact badly on relationships. It can also cause anxiety, depression, and suicidal thoughts. Physical signs can include sleep deprivation, weight gain or loss, skin problems, ulcers, bowel problems, headaches, and muscle pains. A person is likely to suffer withdrawal symptoms and will often lie to cover the extent of the problem. As most people do not admit they have a problem, a major component of treatment is helping them to acknowledge it. The true prevalence of the disorder is not known as so many hide their habit.
☑ TREATMENT
. Cognitive behavioural therapy to help people learn to resist the beliefs and behaviours that maintain the disorder.
. Psychodynamic therapy to help grasp the meaning and consequences of the behaviour.
. Self-help groups and counselling to help understand how the behaviour affects others.
Kleptomania
An individual with kleptomania has an irresistible and repeated compulsion to steal items. These episodes of stealing occur unexpectedly, without planning.
What is it?
A person with kleptomania steals on impulse and often throws the stolen goods away, as they are mostly interested in the act of stealing. Kleptomania is distinguished from shoplifting as most shoplifters plan the theft, usually because they want an item but do not have enough money to buy it.
Many people with kleptomania live secret lives of shame because they are afraid to seek help; up to 24 per cent of those arrested for shoplifting are thought to suffer from it. Kleptomania is associated with other psychiatric problems such as depression, bipolar disorder, generalised anxiety disorder, eating and personality disorders, substance abuse, and other impulse-control disorders. There is evidence to link kleptomania with the neurotransmitter pathways associated with behavioural addictions and mood-enhancing neurochemicals like serotonin.
There is no specific cure for kleptomania, but psychotherapy and/or medication may help break the cycle of compulsive stealing.
Perpetual pattern
A person with kleptomania may report feeling tense before they steal, then pleased, and gratified as they do it. The subsequent guilt can increase the tension again.
☑ TREATMENT
. Psychotherapies such as behaviour modification, family, cognitive behavioural, and psychodynamic therapies to explore the underlying causes and put in place more appropriate ways of dealing with distress.
. Selective serotonin reuptake inhibitors (SSRIs) alongside therapy.
Pyromania
A person with pyromania sets fires purposefully. This very rare impulse-control disorder is triggered by stress, and the action provides relief from tension or distress.
What is it?
Also known as firesetting, pyromania is an obsessive desire to light fires. It can be a chronic (long-term) problem or restricted to several occurrences during a period of unusual stress. A person with pyromania is excessively fascinated by making fires and situations involving fire, as well as witnessing or assisting in the fire’s aftermath.
Individual factors that contribute to pyromania may include antisocial behaviours and attitudes, sensation and/or attention seeking, lack of social skills, and inability to cope with stress. Parental neglect or emotional detachment, parental psychological disorders, peer pressure, and stressful life events can all be triggers both in children and adults. Interviews with affected children and teens often identify a chaotic household, in which case a whole-family approach to treatment is required.
Destructive cycle
. Tension builds up, leading to a strong desire to light a fire.
. Lighting the fire gratifies overwhelming urge.
. Feelings of euphoria and relief result from seeing the fire.
. Fire, its aftermath, and fire-related equipment and personnel fascinate the person.
PYROMANIA IN CHILDREN, TEENS, AND ADULTS
In children and teens firesetting may be a cry for help, or part of a longer pattern of aggression. Teens may be influenced by antisocial adults in their community. Some are diagnosed with psychotic or paranoid disorders, and others may be cognitively impaired.
In adults, pyromania has been linked to symptoms that include depressed mood, thoughts of suicide, and poor interpersonal relationships. It is often associated with psychological problems such as OCD.
☑ TREATMENT
. Cognitive and behavioural therapies tailored for children to include problem-solving and communication skills, anger management, aggression replaceable training, and cognitive restructuring. Long-term, insight-oriented psychotherapy for adults.
DID (dissociative identity disorder)
In this rare and severe condition, a person’s identity is fragmented into two or more distinct personality states. The parts do not join up into a whole.
What is it?
A person with DID has a splintered identity, rather than a growth of separate personalities, which is why the name of the condition was changed from its previous term of multiple personality disorder.
The individual feels as though they have different people within (called alters). Each alter has its own persona, with its own pattern of thinking and communicating, even down to different handwriting and physical requirements, such as wearing glasses. Someone with DID finds it hard to define what they are like and may refer to themselves as “we”. They have no control over when and which alter takes over, and how long for.
Dissociative experiences
An individual with DID uses disassociation – disconnection from the world around them – as a defence mechanism. They may feel as if they are floating away, watching themselves from outside. As if in a film, the person observes rather than feels their emotions and parts of their body. The world around a person affected by DID may seem unreal and hazy, with objects changing appearance.
The individual has significant and frequent gaps in memory, unable to recall personal information in a way that is more extreme than forgetfulness. They may not remember people, places, and events in their lives from the distant and recent past, yet relive other things that have happened vividly. The person has moments of absence while carrying out day-to-day activities and may travel somewhere but be unable to remember how they got there.
The person regularly experiences symptoms of personality change and dissociation. These symptoms are thought to be a way of coping that often goes back to severe and prolonged trauma experienced in childhood, but the dissociation disrupts everyday life long after the trauma has ceased. Affected individuals continue to use the dissociation as a way of coping in all stressful situations in later life.
How is it diagnosed?
If a specialist suspects DID, they will complete mental health questionnaires that capture and rate the person’s symptoms.
The aberrant and inexplicable behaviour that characterises DID is distressing and confusing for the individual and impacts negatively on work, social life, and intimate relationships. DID often exists alongside anxiety and depression, panic attacks, OCD, hearing voices, and suicidal feelings.
Identity alteration
Each alter, as the identity fragments of someone with DID are called, has distinct patterns of perception and personality that recur and take control of the individual’s behaviour. Typically, the personalities know each other and communicate, sometimes criticising one another. The transition from one to another is sudden, and the person has no control over which one is in charge, but certain stressors can make a particular alter emerge.
The typical number of identities in people with dissociative identity disorder ranges from 8 to 13.
Switching between alters
. Another gender or age changes memories or perceptions of events.
. Change of role can enable a view of life events from another standpoint.
. The host identity is the one main alter that a person may feel is most like them. This host identity may not remember facts about their personal history when a different alter is in control.
. Different appearance, for example, hair colour or clothing style, can change the host’s persona.
. Different name can denote a switch to the thinking patterns of another alter.
. A younger self may talk in a childlike way or even be unable to talk.
. Opposing attitude from the host’s identity provides a different perspective on life events.
☑ TREATMENT
. Psychotherapies, such as cognitive behavioural therapy, to reappraise the trauma and develop psychological flexibility to help deconstruct the personalities and reunite them into one. Treatment is long term.
. Dialectical behaviour therapy to treat any self-harming and suicidal behaviours.
. Anti-anxiety medication and antidepressants often prescribed to help the person cope with associated conditions.
Depersonalisation and Derealisation
These are two related dissociative disorders. Depersonalisation makes a person feel disconnected from their thoughts, feelings, and body, while derealisation makes them feel disconnected from their environment.
What are they?
The feelings that result from these two conditions can be very disturbing and seriously interfere with a person’s ability to function. Some people fear they are going mad, or become depressed, anxious, or panicky. People with depersonalisation describe feeling like a robot and not in control of their speech or movement; that they are an outside observer of their own thoughts or memories. They may also feel that their body is distorted. With derealisation a person can feel alienated and disconnected from their surroundings. In some, the symptoms for these disorders are mild and short-lived, whereas in others they may persist for months or even years.
Little is known about what causes these disorders, but biological and environmental factors may play a role. Some people appear to be more prone to them because they are neurologically less reactive to emotions, or they may have a personality disorder. The disorders can be triggered by intense stress, trauma, or violence.
If symptoms are present, a clinical assessment will include a full medical history and physical examination to rule out illness or side effects of medication, and questionnaires will be completed to identify associated symptoms and possible triggers. An individual is only diagnosed with depersonalisation and/or derealisation disorder when they persistently or repeatedly suffer from distorted perceptions of detachment from themselves or their environment. Many people experience a temporary feeling of dissociation from their thoughts or surroundings at some point in their lifetime, but fewer than two per cent of people will be identified as having one, or both, of these disorders.
Out of body experience
A person can be so dissociated from reality that they feel as if they are observing themselves in a movie and cannot relate to the individual in the real world.
☑ TREATMENT
. Psychotherapies, particularly cognitive behavioural therapy, psychodynamic therapy, or mindfulness meditation can help a person understand why the feelings occur, learn coping strategies to manage the situations that trigger them, and gain control over symptoms.
. Medication, such as antidepressants, can be prescribed to treat any associated disorders, including anxiety and depression.
Dissociative amnesia
This is an often short-term, dissociative disorder, in which a person becomes separated from their personal memories following stress, trauma, or illness.
What is it?
Dissociative amnesia is often linked to overwhelming stress, such as witnessing or suffering from abuse, an incident, or a disaster. The resulting severe memory loss often affects specific recollections, such as a certain period during childhood, or something associated with a friend, relative, or peer. Alternatively, the amnesia may focus on a traumatic event, for example, a crime victim may have no memory of being robbed at gunpoint but can recall details from the rest of that day. A person may develop generalised memory loss and may not remember their name, job, home, family, and friends. They may disappear and be reported missing. They might even create a totally new identity, fail to recognise people or places from their past life, and be unable to explain themselves – this is known as dissociative fugue.
Clinical diagnosis will involve completing assessment questionnaires that help identify a trigger and enable the individual to capture and rate their symptoms. Physical checks and psychological examinations are also carried out to exclude other medical causes of memory loss.
Anecdotal evidence suggests that 2–7% of people have dissociative amnesia.
Memory recovery
Most cases of dissociative amnesia are short-term, and while memories may temporarily fall away, they often return suddenly and completely. The recovery may happen on its own, after being triggered by something in the person’s surroundings, or in a therapy session.
☑ TREATMENT
. Psychotherapies, such as cognitive behavioural therapy, dialectical behaviour therapy, eye movement desensitisation and reprocessing, family therapy, art therapies, hypnosis, or mindfulness meditation can help the person understand and deal with the stress that triggered the disorder and learn coping strategies.
. Medication, such as antidepressants, may be prescribed for the depression or psychosis which can be associated with the amnesia.
Anorexia nervosa
With this serious emotional disorder, a person wants to weigh as little as possible. They develop an aversion to food and their appetite reduces as they eat less and less.
What is it?
A person with anorexia becomes so afraid of gaining weight that they cannot eat normally. They may take appetite suppressants, laxatives, or diuretics (to remove body fluid), or make themselves vomit after meals (bulimia nervosa), but they may also binge (binge-eating disorder).
Many factors can trigger anorexia. Pressures at school, such as exams or bullying (particularly if the focus is on body weight or shape), can contribute, as can occupations such as dancing or athletics where being considered thin is considered “the ideal”. The disorder can also be a response to stress in childhood or a lack of control over life events, such as losing a job, relationship breakdown, or bereavement, which makes the person exert excessive control over internal processes that are within their power.
Anorexia affects more females than males. Many of those who develop it share personality and behavioural traits. They are often emotionally controlled, have a tendency towards depression and anxiety, find it difficult to handle stress, and worry excessively. Many individuals set themselves strict, demanding goals. They may have feelings of obsession and compulsion, but not necessarily OCD. Living with anorexia can make it hard to maintain relationships. It can also have an irreversible impact on the body and cause infertility or serious pregnancy complications.
How is it diagnosed?
A medical doctor in general practice, clinical psychologist, or specialist health professional asks the individual questions about their personal and family history, weight, and eating habits. The person needs treatment as early as possible to reduce the risk of complications. In most cases, the treatment plan involves psychotherapy and individually tailored advice on eating and nutrition. Recovery can take years.
Symptoms of anorexia
All symptoms relate to self-esteem, body image, and feelings, and divide into three main categories: cognitive (feelings and thoughts), behavioural, and physical.
46% of people with anorexia recover fully.
Perceived body weight is too high, and the person feels compelled to lose weight.
Cognitive symptoms
. Expresses a fear of gaining weight and becomes obsessed with body shape.
. Believes that being thin is good and is convinced that they are overweight.
. Measures self-worth in terms of body weight and shape.
. Obsesses about food and the perceived negative consequences of eating.
. Becomes irritable, moody, and unable to concentrate (partly due to hunger), which impacts on everyday life.
Actual body weight and BMI are much lower than is healthy for their age and height.
Behavioural symptoms
. Behaves obsessively around food and diets and counts calories excessively. Avoids “fatty” foods and/or eats only low-calorie foods. May skip meals.
. Avoids eating in front of others, and/or purges after eating.
. Lies about how much they eat.
. Repeatedly weighs themselves or checks their body shape in the mirror.
. Exercises obsessively.
. Becomes socially withdrawn.
Physical symptoms
. Obvious weight loss.
. Irregular or absent periods in females.
. Poor dental health and smelly breath due to persistent vomiting.
. Soft, fine, “downy” hair growing on the body, while head hair falls out.
. Has difficulty sleeping but is very tired.
. Is weak, lightheaded, and dizzy.
. Has stomach pains and is constipated and bloated.
. Has swollen hands and feet.
☑ TREATMENT
. Multidisciplinary care team, including a medical doctor from general practice, psychiatrists, specialist nurses, and dieticians to ensure that a person gains weight safely and to support family and close friends.
. Cognitive behavioural therapy, to help the person understand and explain their problem and see it as a cycle of triggers, thoughts, feelings, and behaviours. Therapist and patient collaborate on interventions that break the chain of thoughts maintaining anorexia.
. Cognitive analytic therapy to examine the way the person thinks, feels, and acts, as well as the events and relationships that underlie their past experiences – often in childhood.
. Interpersonal therapy to resolve problems with attachment and relating to other people.
. Focal psychodynamic therapy to explore how early childhood experiences may have affected the person.
. In-patient treatment for severe cases: supervised weight gain through strict daily routines and eating plans, often including group therapy for peer support.
Bulimia nervosa
A serious eating disorder, bulimia is characterised by a person controlling their weight through severely restricting intake, then binge-eating and purging the body of the food.
What is it?
People with bulimia have an abnormal fear of putting on weight and so become obsessed with food and dieting. Unlike those with anorexia, they have a distorted self-image and believe they are too fat.
A person with bulimia may often appear tense or anxious and behave furtively, rapidly consuming large amounts of food in secret before disappearing to the bathroom to make themselves vomit. This behaviour is a mechanism for coping with life events – although in fact it makes daily living a struggle – and is linked to depression, anxiety, and social isolation. Pressure to conform to body shapes promoted by the fashion and beauty industries and a family history of bulimia increase the risk. Bulimia is more common in females, but incidence in males is rising. Puberty and self-consciousness are often triggers, and boys and girls in their teens are especially vulnerable to bulimia if teased or bullied as an overweight child.
Bulimia can cause irreversible damage to the heart, bowels, teeth, and fertility. Treatment depends on the severity of the condition and recovery can be a long process.
Binge-purge cycle
The person has a low self-opinion and sees losing weight as a way of gaining self-worth. They may also exercise fanatically to burn off the additional calories and avoid social occasions that involve food.
Causes:
. The individual may have a caregiver who thinks looks are important and criticises their weight or appearance.
. The person may want to take control of an aspect of their lives, particularly if recovering from a traumatic event.
. Images of celebrities with flawless, thin bodies trigger the start of strict dieting.
. Despair sets in when the person cannot keep to the diet.
The cycle of low self-esteem
Food cravings set in, which before long are irresistible.
Bingeing provides temporary relief from unhappiness.
Purging brings a short-term respite from the fear of gaining weight.
Guilt and shame result from the purging, leading to depression.
A strict diet seems the best solution to avoid weight gain.
Physical effects:
. Frequent weight gain and loss.
. Bad breath, stomach pain, sore throat, and damaged tooth enamel from acid levels in vomit.
. Dry skin and hair, hair loss, brittle nails, lethargy, and other signs of poor nutrition.
. Heart strain, piles, and weak muscles from misuse and overuse of laxatives and diuretics.
. Irregular/absent periods in females.
. Feeling bloated and/or constipated.
. Bloodshot eyes.
. Calluses on the back of hands from induced vomiting.
DIAGNOSING BULIMIA
Medical doctors in general practice in the UK use the so-called SCOFF questionnaire to diagnose anorexia or bulimia. Two or more “yeses” indicate a likely case. Doctors in other countries apply similar criteria.
[1] Does the person makes themselves Sick (vomit) after eating?
[2] Has the person lost Control over how much they eat?
[3] Have they lost more than One stone (6kg) within three months?
[4] Does the person believe they are Fat even though others have told them they are too thin?
[5] Does Food dominate their life?
☑ TREATMENT
. Psychotherapies such as group therapy, self-help, or one-to-one cognitive behavioural therapy or interpersonal therapy.
. Antidepressants prescribed alongside therapy.
. In-patient treatment needed in extreme cases.
Binge-eating disorder
With this condition, a person regularly overeats to cope with low self-esteem and misery, although in fact the persistent, uncontrolled binge-eating makes depression and anxiety worse.
What is it?
A person with binge-eating disorder regularly eats large amounts quickly when not hungry, alone or secretly, and feels shame and self-disgust after a binge. They feel they have no control over how much and how often they eat.
Low self-esteem, depression, anxiety, stress, anger, boredom, loneliness, dissatisfaction with the body, pressure to be thin, traumatic events, and a family history of eating disorders are all factors that increase the risk of developing it. The disorder can also develop after following such a strict diet that the person is left very hungry and has food cravings. It is the most common eating disorder in the US.
A medical doctor in general practice may diagnose the disorder from the person’s weight gain – the most common physical effect.
Bingeing cycle
People with a binge-eating disorder are using food as an instant, albeit negative, way to relieve emotional pain instead of finding positive methods of tackling the underlying cause. The result is a perpetual cycle of eating, relief, depression, and yet more eating.
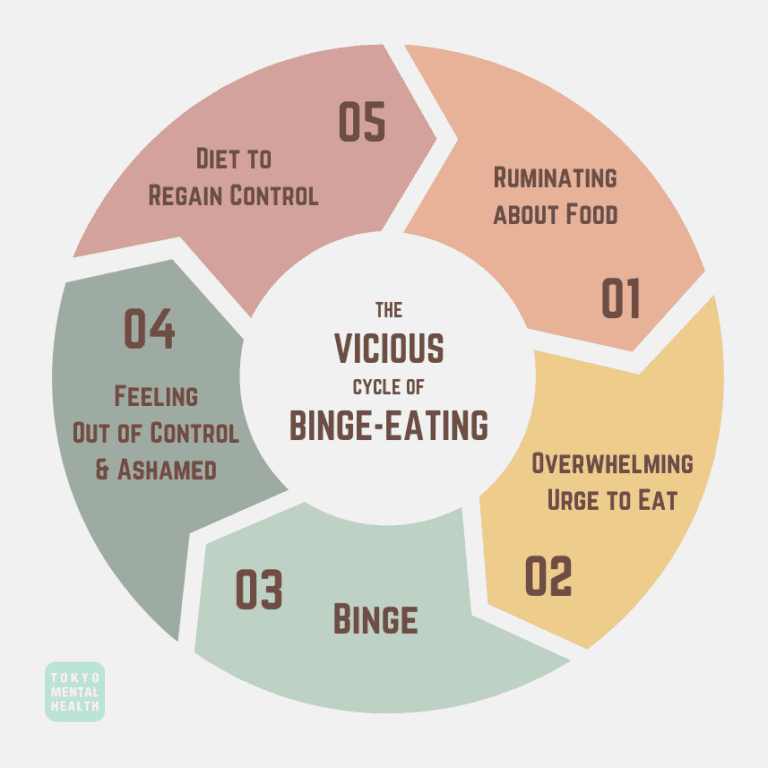
The cycle explained
The person eats large amounts of food rapidly (regardless of degree of hunger), often in secret, may be in a dazed state while eating, and may feel uncomfortably full afterwards.
Anxiety drops as eating temporarily numbs the feelings of stress, sadness, or anger.
Low mood returns with self-disgust because of the guilt and shame associated with binge-eating.
Anxiety rises and depression sets in as eating provides only short-lived “pain” relief.
Relief from increasingly distressing feelings comes only with thoughts of food.
The need to eat to relieve depression grows in urgency: the person plans a binge, often buying special foods for the purpose.
☑ TREATMENT
. Psychotherapy in groups or one to one.
. Self-help programmes through books, online courses, as part of a support group, or supervised by a health professional.
. Antidepressants prescribed alongside therapy.
Pica
An individual with this eating disorder persistently eats substances that are not food, such as dirt or paint. It can lead to serious complications if the substance is dangerous when ingested.
What is it?
Children and adults with pica may eat, for example, animal faeces, clay, dirt, hairballs, ice, paint, sand, or metal objects such as paperclips. It is more common in children than adults – between 10 and 32 per cent of children aged 1–6 years are affected by pica. The odd eating behaviour can create complications such as lead poisoning or intestinal damage from sharp objects. For a medical doctor in general practice to diagnose pica, the pattern of behaviour must last for at least one month. After a medical examination to rule out causes such as nutrient deficiency or anaemia at the root of the unusual cravings, a specialist health professional evaluates the presence of other disorders such as developmental disabilities or OCD.
28% of pregnant women are affected by pica.
☑ TREATMENT
. Behavioural therapies to associate healthy eating with positive reinforcement or reward. Positive behaviour support to address aspects of family and home environment and minimise recurrence.
. Medication to enhance dopamine levels; supplements to remedy any nutrient deficiencies.
RARER EATING DISORDERS
There are rarer eating disorders, namely, purging disorder, night-eating disorder, and rumination disorder. These disorders will not be covered on this site.
Communication disorders
This range of conditions affects a person’s ability to receive, send, process, and/or understand verbal, non-verbal, and visual concepts and may be apparent in hearing, language, and/or speech.
What are they?
The four main conditions are language, childhood fluency, speech-sound, and SCD (social communication disorders). They are often complex. Some are apparent in babies and toddlers, while others may not become obvious until a child is at school.
The causes are wide ranging. Communication disorders may develop of their own accord or stem from a neurological illness. They can be genetic – 20-40 per cent of children with a family history of speech and/or language impairment have communication disorders. Prenatal nutrition may be involved. Psychiatric disorders, ASD (see above), Down’s syndrome, cerebral palsy, and physical problems including cleft lip or palate and deafness may limit a person’s ability to communicate.
How are they diagnosed?
To maximise a child’s development potential, early intervention is important; some conditions require life-long management. A speech and language specialist takes a case history, including information about family background, medical conditions, and information from teachers and carers, to prepare a treatment plan.
[1] LANGUAGE DISORDER
The child does not understand others (receptive disorder) or cannot communicate thoughts (expressive disorder) or both (receptive-expressive disorder).
. Baby does not smile or babble in response to parents, and only has few words by 18 months.
. Child does not play with others and prefers to be alone. May become shy and distant.
. Child has difficulty swallowing, affecting ability to speak.
Causes of language disorder include family history of language impairments, childhood development disorder, genetic syndrome, impaired or no hearing, emotional or psychiatric disorder, premature birth, neurological illness or damage, and poor diet.
[2] CHILDHOOD FLUENCY
The child stutters or stammers, repeating words or parts of words, and prolonging speech sounds.
. Speech can become blocked as if child is out of breath.
. Child uses distracting sounds such as throat clearing or head and body movements to disguise their problem.
. Anxiety is increasingly evident as child tries to hide disorder.
. Child avoids public speaking as the anxiety worsens stammer.
Causes of childhood fluency disorder include a family history of language impairments, childhood development disorder, an emotional or psychiatric disorder, and neurological illness or damage.
[3] SPEECH-SOUND DISORDER
The child has difficulty articulating sound patterns and mispronounces words beyond expected age range.
. Unclear speech, common in young children, continues beyond the age of eight.
. Child unable to produce correct sound patterns even though they can understand speech, so cannot make themselves understood by others.
. Limited understanding of rules of speech sounds is apparent.
Causes of speech-sound disorder include childhood development disorder, genetic syndrome, impaired or no hearing, and neurological illness or damage.
[4] SCD (SOCIAL COMMUNICATION DISORDERS)
The child cannot process verbal and visual information simultaneously.
. Child cannot adapt language to suit situation, so can be dogmatic, dominating, and inappropriate when talking to adults and peers.
. Child lacks non-verbal communication skills such as taking turns in conversation or other group activities.
. Child cannot greet people as has little or no interest in social interaction.
Causes of SCD include a family history of language impairments, childhood development disorder, genetic syndrome, having an emotional or psychiatric disorder, premature birth, neurological illness or damage, and poor diet.
More than one causal factor may be involved in any of the communication disorders, and the effects can range from mild to profound.
IMPACT ON THE CHILD
Errors of thinking and communication affect daily interactions. Children become anxious with low self-confidence.
. Developmental milestones are delayed as children learn through communication.
. Social isolation occurs because child does not initiate interaction and cannot make friends. Many become target of bullies.
. Behavioural issues arise as child adopts avoidance techniques and may become aggressive if they cannot resolve speech difficulties.
SOCIAL COMMUNICATION DISORDER OR AUTISM SPECTRUM DISORDER?
SCD (social communication disorder) has many symptoms in common with ASD (autism spectrum disorder). Assessment must rule out ASD before medical doctors can diagnose the child with SCD and establish a treatment plan.
Social communication disorder – Children with SCD find it difficult to learn the basic rules of conversation; how to start one, listen, phrase questions, stay on topic, and know when it is over. SCD can occur alongside other developmental issues such as language impairment, learning disabilities, speech-sound disorder, and ADHD.
Autism spectrum disorder – Children with ASD find it hard to relate to people, emotions, and feelings. As with SCD, this can result in communication difficulties, impaired social skills, and altered sensory and visual perception. But ASD has an additional defining characteristic of restricted or repetitive behaviours.
☑ TREATMENT
. Speech and language therapy essential to help language skills, speech-sound production and rules, fluency, and non-verbal gestures; for stammerers, support to control and/or monitor rate of speech and breathing.
. Positive behaviour therapies to improve the relationship between behaviour and communication.
. Family therapy, special educational support, and environmental adaptations to support language development.
Sleep disorders
This is a group of conditions that affect a person’s ability to sleep well. Their cause may be psychological or physiological, but they can all result in disturbed thoughts, emotions, and behaviours.
What are they?
Most people experience sleep problems from time to time. The problem becomes a disorder if it occurs regularly and interferes with daily life and mental health. Lack of refreshing sleep can have a negative impact on energy, mood, concentration, and overall health – disorientation, confusion, memory problems, and speech disturbances can result, which may in turn worsen the disorder.
Sleep involves transitions between three different states: wakefulness, REM (Rapid Eye Movement) sleep, which is associated with dreaming, and N-REM (Non-Rapid Eye Movement) sleep. Disorders include abnormal occurrences not only during sleep but also just before sleep and immediately on waking. For example, a person may have difficulty falling and/or staying asleep (insomnia) and then feel extremely tired throughout the day. A person’s sleep may be disturbed by abnormal behaviour or events (parasomnias), such as sleepwalking, nightmares, sleep terrors, restless leg syndrome, sleep paralysis, and sleep aggression. Confusional arousal makes a person behave in a strange and confused way when they wake up. REM sleep behaviour disorder is a severe parasomnia that causes sleep-related groaning, and a person often physically enacts their dreams.
Anecdotal evidence suggests that between 50 and 70 million American adults have a sleep disorder.
What are the causes?
Sleep disruption can be associated with medications, underlying medical conditions (for example, narcolepsy), and sleep-related breathing conditions. The latter includes a range of anomalies from snoring to obstructive sleep apnoea (a condition in which the walls of the throat relax and allow narrow sleep, interrupting normal breathing), which causes the person to wake up in distress.
[1] Insomnia is difficulty in getting to sleep and/or staying asleep long enough to feel refreshed the next day. Episodes can be short-lived or continue for months or years. It is more common in older adults.
Causes – Triggers include worry and stress, for example, problems at home or work or financial difficulties; a significant event, such as a bereavement; underlying health conditions; and alcohol or drug use.
Symptoms – The person may have trouble falling asleep; wake often during the night; wake early and not go back to sleep; and be unable to even nap. Tiredness causes irritability, anxiety, and poor concentration.
Impact – The person cannot relax, and excessive fatigue limits daytime activities. Work performance is impaired, and relationships suffer. Bedtime can be anxiously anticipated, the stress worsening the insomnia.
✔ Treatment – Stimulus-control or sleep-restriction therapies and paradoxical intention and behavioural therapies – the person tries to stay awake for as long as possible to reduce anxiety around sleep.
[2] Parasomnias are a group of unwanted events, experiences, or behaviours that occur while a person is falling asleep, sleeping, or waking. The person remains asleep throughout and has no memory of them.
Causes – Parasomnia often runs in families, so it may be genetic; it is associated with medication or physical conditions such as sleep apnoea; REM sleep behaviour disorder can follow a brain disease.
Symptoms – Common symptoms are sleepwalking; sleeptalking; night terrors; confusional arousal; rhythmic movement; and leg cramps. More severe are night-eating disorder and REM sleep behaviour disorder.
Impact – The lack of refreshing sleep can result in mental impairment, disorientation, confusion, and memory problems. Those with REM sleep behaviour disorder can become violent.
✔ Treatment – Mild or harmless parasomnias need only practical safeguards such as removing possible sources of injury to sleepwalkers. Medication may be needed for REM sleep behaviour disorder.
[3] Narcolepsy is a long-term disorder that can develop if the brain is unable to regulate sleeping and waking. It is characterised by irregular sleep patterns and suddenly falling asleep at inappropriate times.
Causes – Narcolepsy may be genetic or caused by a lack of melatonin (the brain chemical that regulates sleep); hormonal changes in puberty or menopause; or stress. It can follow infection or inoculation.
Symptoms – include daytime sleepiness; sleep attacks; temporary loss of muscle control in response to emotions such as laughing (cataplexy); sleep paralysis; hallucinations on falling asleep or before waking.
Impact – Narcolepsy disrupts daily life and can be difficult to cope with emotionally. An underactive thyroid gland, and other physical symptoms such as sleep apnoea or restless legs, can exacerbate problems.
✔ Treatment – Adopting a healthy lifestyle and diet, regular bedtime routines, and evenly spaced naps to manage excessive daytime drowsiness can all help.
[4] Hypersomnolence is excessive sleepiness that intrudes on daily functions. It can be mild and transient, or persistent and severe, and it often accompanies depression. It mostly affects teens and young adults.
Causes – Hypersomnolence may be genetic; due to drug or alcohol abuse or other sleep disorders such as narcolepsy or sleep apnoea; it can follow a tumour, head trauma, or injury in the central nervous system.
Symptoms – The person may be very sleepy during the day despite night-time sleep of at least seven hours; have recurrent daytime naps or sleep lapses; struggle to wake up after a long sleep; or feel unrefreshed after sleeping for 14-18 hours.
Impact – The person struggles to function in daily life. They may be anxious, irritable, and restless, and have little appetite and no energy. Thinking and speech are slow, and memory problems can develop.
✔ Treatment – Physical causes are treated first. If hypersomnolence persists, daytime activity is observed. Tailored behavioural therapies include introducing pre-sleep routines and ordered sleep times, which are then altered gradually.
Tic disorders
Tics are sudden, painless, non-rhythmic behaviours that are either motor (related to movement) or vocal. A disorder may be diagnosed when tics occur repeatedly and are apparently unconnected to the environment or situation.
What are they?
Tics – small, uncontrollable movements or sounds – are not usually serious and normally improve over time. However, if they persist, they can be frustrating and interfere with everyday activities – especially if the person has more than one tic.
Changes in parts of the brain that control movement are thought to cause tics. There is probably a genetic predisposition too. Taking drugs such as amphetamines or cocaine can trigger tics, as can medical conditions, including cerebral palsy and Huntington’s disease, or psychological disorders such as ADHD and OCD.
Tics are more common in children, but they can begin in adulthood. Statistics vary regarding the prevalence, with 0.3–3.8 per cent of children described as having severe tics. Treatment may not be needed if a tic is mild; lifestyle management, such as avoiding stress or tiredness, is often all that is required.
ADVANCE WARNINGS
Most people have an unusual or uncomfortable feeling before the tic occurs. Individuals often describe this as a rising tension that only the tic itself can release. Some people can suppress their tics for a short period, until the urge to do it becomes too strong which may result in a more severe tic.
Warning urges include a burning sensation behind the eyes, tension in a particular muscle, dry throat, and itching.
Simple and complex tics
Tics take many forms. Some affect body movement and others are verbal. They may be simple or complex. A simple tic affects a small number of muscle groups, for example, blinking or clearing the throat. A complex tic involves coordinated patterns of several muscle groups, such as blinking in combination with a shoulder shrug, facial grimace, and spontaneous shouting.
Motor tics include grimacing – head jerking – head banging – shoulder shrugging – eye blinking – nose twitching and sniffing – twisting of the body – tensing of the abdomen – clicking fingers – touching objects or people.
Vocal tics include throat clearing – coughing – grunting – frequent spitting – making animal noises – hissing at people – loud swallowing.
Palilalia (repeating own words or phrases), Echolalia (repeating the words of other people), and coprolalia (uttering obscenities) are also likely to occur.
TOURETTE’S SYNDROME
This is a condition characterised by multiple tics, named after George de la Tourette, who first described it in 1884. For a condition to be classified as Tourette’s syndrome, the tics must last for at least a year and at least one must be vocal. Most individuals have a combination of motor and vocal tics, which can be both simple and complex. The syndrome often runs in families.
Tourette’s syndrome is thought to be linked to problems with a part of the brain called the basal ganglia or possibly to a childhood sore throat infection caused by a streptococcal bacteria. The first stage of diagnosis is to check other possible causes of the symptoms such as allergies or poor eyesight. A neurologist or psychiatrist then rules out conditions such as ASD before referring the person for psychotherapy. In a third of cases, the tics reduce, become less troublesome, or disappear over a 10-year period.
☑ TREATMENT
. Behavioural therapies are widely used for Tourette’s to expose the unpleasant feelings that precede the tic and encourage a response that stops it.
. Habit reversal training to teach use of incompatible behaviours in place of the tic, so planned intentional movements compete with the tic and prevent it.
. Lifestyle management such as relaxation techniques and listening to music to reduce frequency of tics.
. Antidepressants or anti-anxiety medication to support behavioural interventions if needed.
PD (personality disorders)
These are disorders in which individuals display persistent and consistent unhealthy patters of thinking, behaviour, and social functioning.
What are they?
Individuals with PD have difficulty not only understanding themselves, but also relating to other people. PD is different from other mental illnesses due to its enduring nature and the fact that it cannot be compared to a physical illness. The individual’s behaviour varies noticeably from the norm in society, but they may manage their own life without medical help, in a way that someone with an extreme condition such as schizophrenia cannot. PD often goes hand in hand with substance abuse, depression, and anxiety.
The precise causes of personality disorders are not known, but risk factors appear to include a family history of a personality or other mental disorder; an abusive, unstable, or chaotic early life; or a diagnosis of severe aggression and disobedience in childhood. Variations in brain chemistry and structure may also play a role.
There are 10 defined PDs, and they are considered to fit into three clusters based on broad similarities within each group.
A medical doctor in general practice does not usually attempt a diagnosis of PD until early adulthood. For a diagnosis to be made, the symptoms must cause day-to-day problems with functioning, subjective distress, and the person must display some symptoms of at least one of the types.
Cluster A: odd/eccentric
A person with a Cluster A personality disorder shows patterns of behaviour that most onlookers would regard as odd and eccentric, has difficulty relating to other people, and fears social situations. The individual may not believe that they have a problem. This group includes three personality disorders: paranoid, schizoid, and schizotypal.
Paranoid PD
. The person is extremely distrustful and suspicious.
. They think other people are lying to them, trying to manipulate them, or passing on shared confidences.
. They find hidden meanings in innocent remarks.
. They have problems maintaining close relationships, often believing that a spouse or partner is unfaithful, despite a lack of evidence, for instance.
. Their suspiciousness and hostility may be expressed in overt argumentativeness, recurrent complaining, or by quiet, hostile aloofness.
. The person’s hypervigilance for potential threats makes them appear guarded, secretive, devious, and lacking in tender feelings.
Schizoid PD
. The person appears cold, detached, and indifferent to other people.
. They prefer to take part in activities alone.
. They have little desire to form close relationships of any kind, including sexual ones.
. They have a limited range of social expression.
. They cannot pick up social cues or respond to criticism or praise.
. They have limited ability to experience pleasure or joy.
. They are more likely to be male than female.
. They may have a relative with schizophrenia, but schizoid PD is not as severe a condition.
Schizotypal PD
. The person becomes very anxious and introverted in social situations, even familiar ones.
. They make inappropriate responses to social cues.
. They have delusional thoughts, attaching undue and misguided significance to everyday events. For example, they may be convinced that a newspaper headline contains secret messages for them.
. They may believe in special powers such as telepathy or their own magical ability to influence another person’s emotions and actions.
. They may have unusual ways of speaking, such as making long, rambling, vague statements or changing the subject partway through.
☑ TREATMENT
. Paranoid PD Schema-focused cognitive therapy to enable links between problems, for example, emotions from childhood memories and current life patterns; also uses cognitive techniques to develop new appraisals; however, high drop-out rates from treatment occur, even if sought, due to difficulty in building rapport and trust between therapist and patient.
. Schizoid PD Cognitive behavioural therapy or lifestyle support to reduce anxiety, depression, angry outbursts, and substance abuse; social skills training; medication prescribed for low mood or psychotic episodes; however, treatment is rarely sought.
. Schizotypal PD Long-term psychotherapy to build a trusting relationship and cognitive behavioural therapy to help with identification and re-evaluation of irrational thoughts; medication prescribed for low mood or psychotic episodes.
Cluster B: dramatic/emotional/erratic
A person suffering from Cluster B personality disorder struggles to regulate their feelings. They are usually overly emotional and unpredictable and display behaviour patterns that others see as dramatic, erratic, threatening, and even disturbing. This creates a vicious circle, as people are uncomfortable near them, so social and personal relationships are difficult to achieve and maintain, which in turn intensifies the initial symptoms.
PSYCHOPATHY
Sometimes considered a subset of antisocial personality disorder, psychotherapy is one of the most difficult disorders to diagnose and is largely resistant to treatment. Psychopathy presents as a specific set of personality traits and behaviours. Mental Health professionals can use Robert Hare’s Psychopathy Checklist-Revised (PCL-R) to diagnose the disorder by scoring an individual on 20 listed traits with a value of 0, 1, or 2. A score of 30 or above in the US, or 25 and above in the UK, results in a diagnosis of psychopathy. Interpersonal traits include grandiosity, deceit, and arrogance; emotion-based traits, lack of guilt and empathy; and impulsive traits, sexual promiscuity as well as criminal behaviours such as stealing. Individuals lack inhibition and do not learn from experience. They can seem charming at first, but their inability to feel guilt, empathy, or love, along with the presence of casual, reckless attachments and behaviour, quickly becomes evident. Many traits – especially the ability to make clear, emotion-free decisions – can be found in successful individuals, particularly in business and sport. Most psychopaths are men, and the disorder is unrelated to the society or culture they come from.
Antisocial PD
. The person manipulates, exploits, or violates the rights of others.
. They see other people as vulnerable and may intimidate or bully them without remorse. They can be aggressive, even violent.
. Their behaviour is often criminal; they lie and steal and use aliases to deceive people.
. They disregard their own and others’ safety.
. They are consistently irresponsible and impulsive and have no concern for the consequences of their actions.
. They blame other people for problems they encounter.
. The disorder becomes evident in late teens and often dissipates by middle age.
Borderline PD
. The person has a fragile self-image.
. They are emotionally unstable (also called affect dysregulation), with severe mood swings and frequent, intense displays of anger.
. They have intense but unstable relationships with other people.
. They fear being alone or abandoned and have long-term feelings of emptiness and loneliness, leading to irritability, anxiety, and depression.
. They have disturbed patterns of thinking or perception (called cognitive or perceptual distortions).
. They act impulsively, with a tendency to self-harm. Suicidal thoughts may also be present.
Histrionic PD
. The person is self-centred and regularly seeks attention.
. They dress or behave inappropriately and draw attention to themselves through physical appearance.
. Their emotional states rapidly shift, which makes them appear shallow.
. They are excessively dramatic, with exaggerated displays of emotion.
. They constantly seek reassurance or approval.
. They are suggestible (easily influenced).
. They believe that their relationships are more intimate than they are.
. They may function at a high level in social and work environments.
Narcissistic PD
. The person has an exaggerated sense of self-importance, expects to be recognised as superior, and exaggerates their talents.
. They are preoccupied with fantasies about success, power, brilliance, beauty, or the perfect partner.
. They believe they can only associate with people of equal importance.
. They expect special favours and unquestioning compliance from others and take advantage of them to get what they want.
. They are unwilling and unable to recognise anyone else’s needs and feelings.
. They believe they are envied.
☑ TREATMENT
. Antisocial PD Cognitive behavioural therapy: however, person may only seek help when ordered to do so by a court of law because of their criminal behaviour.
. Borderline PD Dialectical behaviour and mentalisation-based therapies combining psychodynamic, cognitive behavioural, systemic, and ecological approaches, and art therapy. Group psychotherapy if symptoms are mild; coordinated care programme for moderate to severe symptoms.
. Histrionic PD Supportive and solution-focused psychotherapy to enable emotion regulation; however, treatment is difficult as individual often exaggerates ability to function.
. Narcissistic PD Psychotherapy to help the person understand the cause of their emotions and regulate them.
Cluster C: anxious/fearful
This group of personality disorders is characterised by worried, fearful thinking or behaviour. A person with one of these disorders struggles with persistent and overwhelming feelings of fear and anxiety and may show patterns of behaviour that most people would regard as antisocial and withdrawn. Cluster C includes dependent, avoidant, and OC (obsessive compulsive) PDs. A psychiatric assessment is needed to differentiate between dependent and borderline PD, as the two share some symptoms.
Dependent PD
. The person fears being on their own and having to fend for themselves.
. They constantly try to please and avoid disagreeing with people, as they are afraid of disapproval.
. They are oversensitive to criticism and pessimistic in outlook.
. They lack self-confidence, suffer from self-doubt, belittle their abilities and assets, and may describe themselves as “stupid”.
. They display needy, submissive, and clinging behaviour, and may tolerate abuse.
. If a close relationship fails, they urgently seek another one.
. They are often unable to start tasks for fear of failure.
Avoidant PD
. The person fears disapproval, criticism, or rejection so strongly that they find it difficult to make connections with people.
. They are extremely cautious in creating friendships.
. They are reluctant to share personal information or feelings, which can make it difficult to maintain the relationships they do have.
. They avoid any work activities that involve interpersonal contact.
. They stay away from social situations because they strongly believe they are inadequate and inferior.
. They worry constantly about being “found out” and others rejecting, ridiculing, or shaming them.
Obsessive compulsive PD
. The person is preoccupied with orderliness, perfectionism, and mental and interpersonal control.
. They are rigid and stubborn in pursuit of their principles.
. They are so devoted to work that they neglect friends and other activities, so they do not form or maintain meaningful social relationships.
. They are over-conscientious and scrupulous and may miss work deadlines because they persistently aim for perfection.
. They are inflexible on matters of morality or ethics.
. They are unable to discard worn-out or worthless objects even when they have no sentimental value.
OCPD OR OCD?
The need to perform behavioural or thinking tasks to reduce the frequency and intensity of obsessional thoughts and compulsions that cause extreme anxiety characterises both OCPD (obsessive compulsive personality disorder) and OCD (obsessive compulsive disorder). However, OCPD begins in early adulthood, whereas OCD can develop at any life stage.
OCPD is an exaggeration of a personality style, and becomes a problem that interferes with daily life, whereas OCD is underpinned by an inflated sense of responsibility for harm occurring to the self or others.
People with OCPD believe their thinking is entirely rational. Those with OCD are aware that their thinking is disordered and that the cycle maintains their anxiety.
☑ TREATMENT
. Dependent PD Psychotherapy, specifically assertiveness training to help with self-confidence, and cognitive behavioural therapy to help develop more robust attitudes and perspectives about themselves relative to others. Long-term psychodynamic therapies to examine early developmental experiences and help rebuild personality.
. Avoidant PD Psychodynamic therapy or cognitive behavioural therapy to help the person identify strongly held beliefs about themselves and how they think others see them and to change behavioural and social skills to improve work and social life.
. Obsessive compulsive PD Counselling and psychotherapy tailored to address every aspect of a person’s strongly held beliefs, in particular, their rigid and entrenched view of the world and others. Cognitive behavioural therapy and psychodynamic therapy to help the person identify their feelings about a situation, then stop to think about why the control maintains, rather than solves, the problems.
Anecdotal evidence suggests that ten per cent (10%) of the global population are affected by some form of personality disorder.
Other disorders
There are a number of conditions with physiological, developmental, or cultural origins that can also have a negative effect on a person’s cognitive and behavioural functioning.
What are they?
There are many physical conditions that affect a person’s performance, limit function, and cause enough distress to trigger behavioural problems as well as depression and anxiety. These include developmental problems (such as Down’s syndrome), physiological conditions (such as dyspraxia, which affects co-ordinated movement), and degenerative illnesses (such as Parkinsonism). Even though not of psychiatric origin, the impairment or distress can be severe enough to require treatment.
Some disturbances are culturally specific, such as Koro or Amok, or arise from a conflict between an individual and their society or culture. Some Western disorders have Eastern counterparts and vice versa, for instance, the Japanese condition Taijin Kyofusho is similar to social anxiety disorder.
Psychological disorders that have been excluded from this page include excoriation and trichotillomania (skin-picking and hair-pulling disorders) and the rarer eating disorders (purging, night-eating, and rumination disorders).
(1)
Somatic symptom disorder is an excessive focus on physical symptoms such as pain or fatigue that causes severe anxiety. The individual will have problems with functioning.
Symptoms – The person will have high levels of anxiety and will panic about the physical symptoms which they believe indicate serious illness.
Possible causes – Genetics; emotional sensitivity to pain; negative personality traits; learned behaviours; problems processing emotions.
Impact – Obsession with negative causes; problems with relationships; poor health; depression; distrust of medical opinion.
✔ Treatment – Cognitive behavioural therapy to examine unhelpful thoughts and behaviours that maintain concern.
(2)
Munchausen’s syndrome (factitious disorder) is where an individual fabricates symptoms, or presents others as ill, injured, or impaired. They do so to gain medical attention.
Symptoms – The person or caregiver deceptively mimics, causes, or exaggerates physical symptoms, and seeks treatment from many doctors.
Possible causes – Combination of psychological factors, stressful experiences, or complex or traumatic relationships in childhood.
Impact – Deception impacts on social relationships; serious health-related problems from unnecessary medical interventions.
✔ Treatment – Psychotherapy to build personal insights and find alternative ways to cope with stress and anxiety.
(3)
Down’s syndrome is a developmental disorder that has varying impact on intellectual, physical, and social functioning.
Symptoms – The individual may have generalised anxiety disorder, OCD, sleep disorders, ADHD in children, and autism spectrum disorder.
Possible causes – Chromosomal abnormality, in which all or some cells in the body contain an extra copy of chromosome 21.
Impact – Mild to moderate cognitive impairment; short- and long-term memory loss; slow acquisition of physical and language skills.
✔ Treatment – Parental support and training, together with early intervention with techniques that support child’s development.
(4)
Gender dysphoria is a conflict that results from a mismatch between a person’s biological sex and the gender they identify with.
Symptoms – Displays feelings and behaviours of the opposite sex, distressed by puberty; disgusted with own genitals.
Possible causes – Probably hormonal influences before birth and intersex conditions (reproductive anatomy not fully male or female).
Impact – Stress; depression and anxiety; self-harm; suicidal thoughts.
✔ Treatment – Psychotherapy to support living in a preferred gender identity; physical transitioning with surgical intervention.
(5)
Sexual dysfunction Men or women experience physical or psychological difficulties that prevent them from enjoying sexual activity.
Symptoms – Men have erectile dysfunction; premature or retarded ejaculation. Women lack desire or have pain on intercourse (dyspareunia).
Possible causes – Physical causes including illness, medication, and substance abuse; stress; performance anxiety; and depression.
Impact – Loss of confidence; social anxiety; low self-esteem; depression; anxiety; panic attacks.
✔ Treatment – Specific interventions for physical problems; couple-based anxiety and stress management; sex therapy.
(6)
Koro (Genital retraction syndrome) is a delusional disorder in which a person has an irrational fear that their genitals are retracting or disappearing.
Symptoms – Strongly believes that penis (nipples in women) is shrinking despite lack of evidence, and that this is a sign of death.
Possible causes – Presence of other mental disorders; lack of psychosexual education in puberty.
Impact – Deep shame; fear; secretive behaviour; depression; anxiety.
✔ Treatment – Psychotherapy and medication for associated depression; treatments as for body dysmorphic disorder and schizophrenia.
This concludes the narrative for the page ‘Applied Psychology (2)’. Amendments to the above entries may be made in the future.

